US Quiz of the Month – Julho 2022
CASE REPORT
The authors present the case of a 33-year-old female patient with dyspepsia. An esophagogastroduodenoscopy was performed (fig. 1). In the second portion of the duodenum (D2), a 15 mm bulge with normal mucosa, non-pulsatile, soft consistency, without pillow sign was observed.
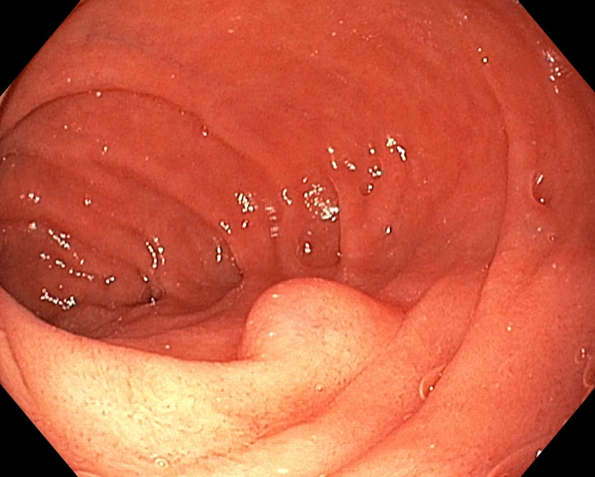
Figure 1. Esophagogastroduodenoscopy (D2): a non-pulsatile 15 mm bulge with normal mucosa and soft consistency.
Endoscopic ultrasonography (EUS) revealed a well-defined hypoechoic nodule arising from the second layer of the duodenal wall, measuring 11 x 4 mm (fig. 2). The nodule echotexture was homogenous, with no calcifications or lymphadenopathies.
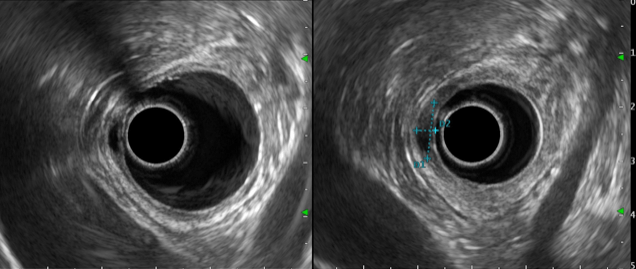
Figure 2. Radial EUS (D2): a well-defined hypoechoic homogeneous nodule arising from the second layer of the duodenal wall, measuring 11 x 4 mm.
QUIZ - WHAT IS THE MOST LIKELY DIAGNOSIS?
DISCUSSION
These findings were compatible with Brunner’s gland hyperplasia. An endoscopic mucosal resection was performed. Histopathological analysis revealed cystic Brunner glands, with no dysplasia or neoplasia. A final diagnosis of Brunner’s gland hyperplasia was made.
Brunner’s gland hyperplasia (BGH), also referred in the literature as Brunner’s gland adenoma and hamartoma, consists of a hyperplastic proliferation of mature Brunner’s glands [1,2]. These are acinotubular exocrine glands located in the submucosal layer of the duodenum that secrete mucin, an alkaline fluid that protects the duodenum from gastric acidity [2]. BGH is a rare lesion, comprising less than 1% of gastrointestinal neoplasms [1]. They usually present as an incidental finding, however occasionally they may be large in size and cause obstruction or bleeding [2,3,4].
Endoscopically BGH may present as a polyp or subepithelial lesion, and the ultrasonographic findings are variable: located mainly in the submucosal layer or extended to the mucosal layer (third and second EUS layers, respectively); variable echogenicity; solid, large, or small cystic; round and well-circumscribed [5]. Although it has generally been considered a benign lesion, there are a few cases reported in the literature where dysplasia and malignant transformation occurred, and therefore endoscopic resection can allow for diagnosis and exclude malignancy [2,6].
REFERENCES
- Requena DO, Rojas C, Garcia-Buitrago M. Cytological diagnosis of Brunner’s gland adenoma (hyperplasia): A diagnostic challenge. Diagn Cytopathol. 2021;49(6):E222-E225.
- McCafferty J, Tokhi A, Krishnamoorthy S, Pande G. Case report of Brunner’s gland hyperplasia: A rare “mimic” of malignant pathology. Int J Surg Case Rep. 2021;81:105827.
- Lazaridis N, Murino A, Solonos F, et al. Saline-immersion therapeutic endoscopy (SITE) combined with endoscopic submucosal dissection (ESD) of a rare cause of intussusception: a giant Brunner gland adenoma. Endoscopy. 2021;53(2):E62-E64.
- Dhouha B, Ahlem L, Sana BS, et al. Brunner’s gland hyperplasia: A rare cause of gastrointestinal bleeding. Pathologica. 2017;109(4):414-417.
- Lee KJ, Park B, Kim HM. Endoscopic Ultrasonography Findings for Brunner’s Gland Hamartoma in the Duodenum. Clin Endosc. 2022;55(2):305-309
- Ramay FH, Papadimitriou JC, Darwin PE. Brunner’s Gland Adenoma with High-Grade Dysplasia. ACG Case Rep J. 2018;5:e81.
AUTHORS
Diogo Bernardo Moura1, Nuno Nunes, Carolina Chálim Rebelo1, Francisca Côrte-Real1, Maria Antónia Duarte1.
- Gastroenterology Department, Hospital do Divino Espírito Santo de Ponta Delgada, Ponta Delgada, Portugal.


