US Quiz of the Month – April 2022
CASE REPORT
A 40-year-old woman with rectal bleeding underwent a colonoscopy. Her past medical history included dysmenorrhea controlled with a hormonal intrauterine device. Colonoscopy revealed a 15 mm polypoid lesion covered by eroded mucosa and luminal narrowing at 20 cm from the anal verge (Fig. 1A and 1B).
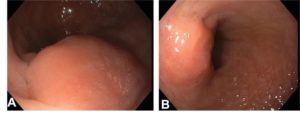
Figure 1. Colonoscopy revealing a 15 mm polypoid lesion covered by eroded mucosa and luminal narrowing at 20 cm from the anal verge.
Histopathologic assessment of standard biopsy specimens was inconclusive. A pelvic magnetic resonance imaging demonstrated a 20 mm neoplastic lesion at sigmoid colon with endophytic growth. An endoscopic ultrasound (EUS) showed a 19×8 mm hypoechoic, round, well-demarcated lesion arising from the muscularis propria and involving superficial layers (Fig. 2).
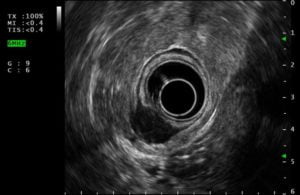
Figure 2. Radial endoscopic ultrasound (EUS) showing a 19×8 mm hypoechoic, round, well-demarcated lesion arising from the muscularis propria and involving superficial layers.
A EUS-guided fine-needle biopsy (EUS-FNB) was performed (Acquire 22 G needle, Boston ScientificTM, 2 passes) (Fig. 3).

Figure 3. A linear EUS-guided fine-needle biopsy (EUS-FNB) performed with Acquire 22 G needle (Boston ScientificTM), 2 passes.
WHAT IS THE MOST LIKELY DIAGNOSIS?
DISCUSSION
Histopathological and cytological examination showed endometrial glands and stroma (Fig. 4), a pattern compatible with endometriosis. The patient is receiving treatment with monthly subcutaneous injection of gonadotropin-releasing hormone agonists.
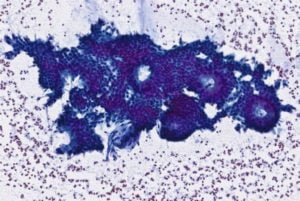
Figure 4. Histopathological and cytological examination of the specimen showing endometrial glands and stroma.
The most common location of extragenital endometriosis is the bowel. Rectosigmoid colon is involved in up to 93% of these cases. Patients may be asymptomatic or may present with dysmenorrhea, hematochezia, lower abdominal pain, constipation, diarrhea, tenesmus, and even bowel obstruction. An association of symptoms with the menstrual cycle is an important diagnostic clue (1). Endoscopically, bowel endometriosis may mimic subepithelial and neoplastic lesions as well as inflammatory, infectious or ischemic disease (2). Standard biopsies obtained during endoscopy are rarely sufficient for the diagnosis and imaging tests are not sensitive for the diagnosis. EUS features of rectosigmoid endometriosis have been reported as including a hypoechoic deep pelvic mass with an irregular or unclear margin infiltrating the anterior wall of the rectosigmoid colon (3). However, to confirm a diagnosis of rectosigmoid endometriosis, histologic identification of endometrial glands and stroma is required. Laparoscopy with direct visualization and tissue sampling is the gold standard for definitive diagnosis. As in our case, EUS-FNB/FNA allows evaluation of lesion characteristics and tissue acquisition for definite diagnosis, avoiding more invasive diagnostic procedures. Therapy choice, medical or surgical, depends on nodules size, location, severity of symptoms and desire of the patient to conceive
REFERENCES
- Shi B, Sun B, Zhao Q, Zhang X. EUS diagnosis of rectal endometriosis. VideoGIE. 2021;6(2):105-7.
- Foulon A, Pichois R, Sabbagh C, Fumery M. Bowel Endometriosis Mimicking Crohn Disease. Inflamm Bowel Dis. 2021;27(3):e26-e7.
- James TW, Fan YC, Schiff LD, Gangarosa LM. Lower endoscopic ultrasound in preoperative evaluation of rectosigmoid endometriosis. Endosc Int Open. 2019;7(6):E837-e40.
- Abrão MS, Petraglia F, Falcone T, Keckstein J, Osuga Y, Chapron C. Deep endometriosis infiltrating the recto-sigmoid: critical factors to consider before management. Hum Reprod Update. 2015;21(3):329-39.
- Habib N, Centini G, Lazzeri L, Amoruso N, El Khoury L, Zupi E, et al. Bowel Endometriosis: Current Perspectives on Diagnosis and Treatment. Int J Womens Health. 2020;12:35-47.
AUTHORS
Mafalda João1, Daniel Brito1, Susana Alves1, José Paulo Magalhães2, Ana Teresa Cadime1
- Gastroenterology Department, Portuguese Oncology Institute of Coimbra.
- Pathology Department, Portuguese Oncology Institute of Coimbra.


