US Quiz of the Month – August 2020
CASE REPORT
We present the case of a 71-year-old female patient with past medical history remarkable for a pancreatic head cystic lesion diagnosed in 2009. It was a 24mm multilocular cystic lesion with a central scar, that remained asymptomatic and stable in size until 2015, when follow-up was lost.
In 2019 the patient developed new onset jaundice, choluria and acolia. An abdominal ultrasound was performed and revealed a 47x45mm heterogeneous mass in the pancreatic head, associated with de-novo common bile duct dilatation (CBD, 17mm in the liver hilum) (Fig. 1).
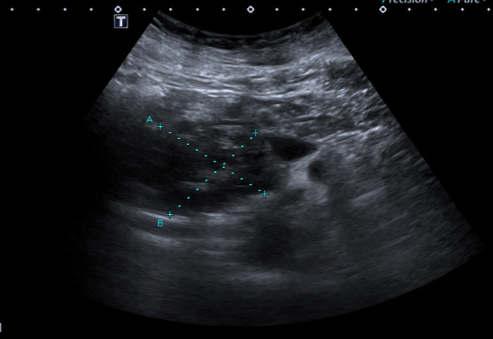
Figure 1. Abdominal ultrasound: heterogeneous pancreatic head mass.
Magnetic resonance cholangiopancreatography (MRCP) showed a multilocular pancreatic head cystic lesion, measuring 60x70x57mm (Fig. 2) and apparently communicating with the main pancreatic duct (MPD). There was also CBD and intrahepatic bile duct dilation.
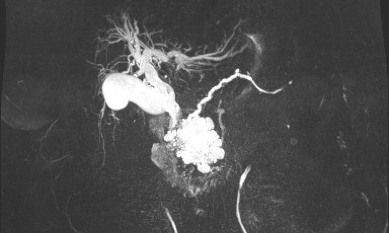
Figure 2. MRCP: multilocular pancreatic head cystic lesion, apparently communicating with the MPD, and CBD and intrahepatic bile duct dilation.
Endoscopic ultrasound (EUS) documented a predominantly microcystic lesion located in the head of the pancreas, measuring 53x46mm, with a few macrocysts and pseudo-solid areas, compressing the CBD and the superior mesenteric vein, and without vascular invasion or Wirsung dilatation (Fig. 3). Fine needle aspiration (FNA) of the macrocyst and of a pseudo-solid area was performed. Cyst fluid biochemistry analysis revealed a high amilase level (54085 UI/L) and a normal CEA (2 ng/mL).
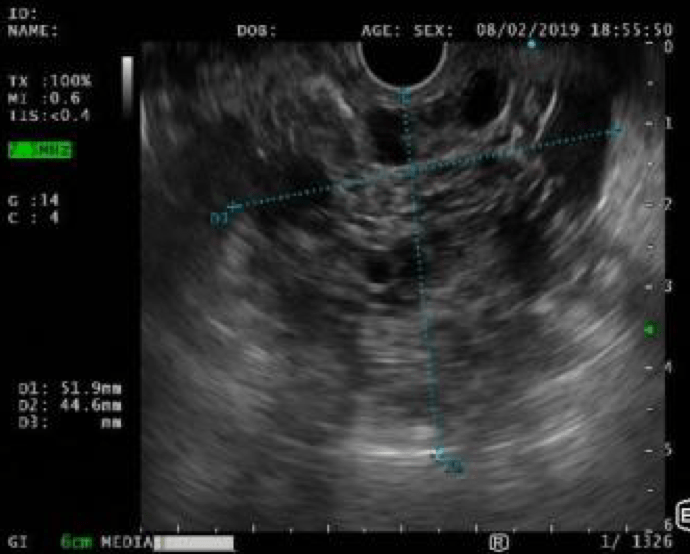
Figure 3. EUS: predominantly microcystic pancreatic lesion located in the head of the pancreas, with a few macrocysts and pseudo solid areas.
WHAT IS THE MOST LIKELY DIAGNOSIS FOR THE PANCREATIC MASS?
DISCUSSION
EUS-FNA cytology showed cuboidal cells, negative for CK8/18, synaptophysin and chromogranin-A, consistent with the diagnosis of a serous cystadenoma (Fig. 4).
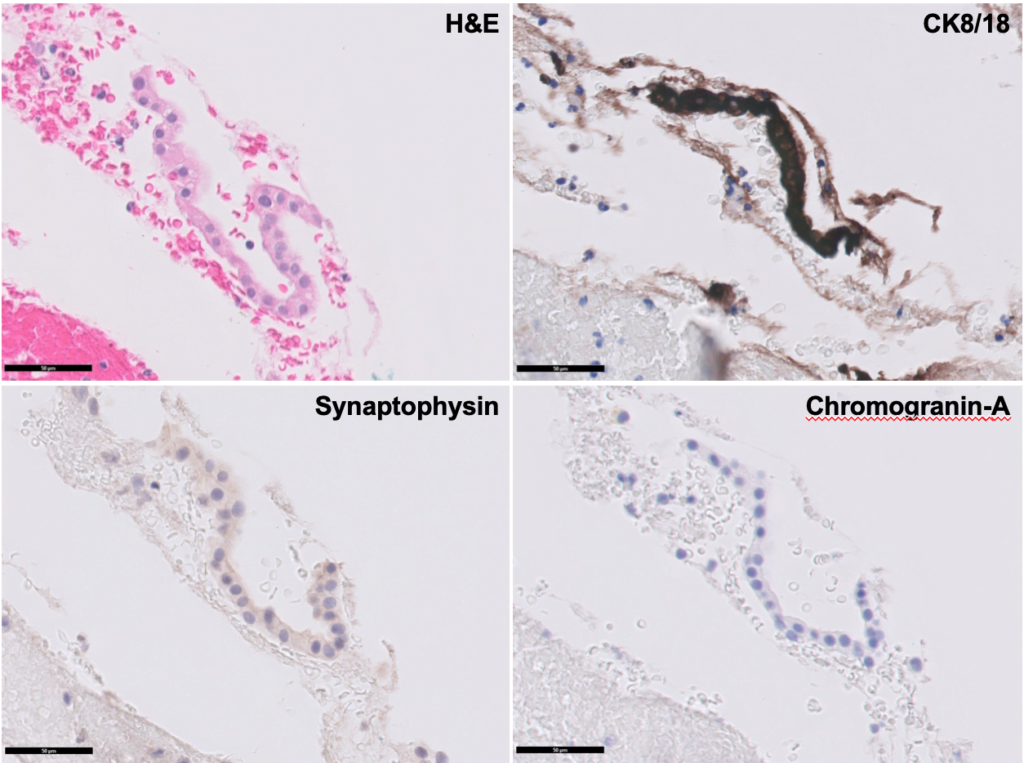
Figure 4. Cytology (x400): cuboidal cells, negative for CK8/18, synaptophysin and chromogranin-A.
ERCP was then performed. Pancreatography showed a multicystic lesion in the head of the pancreas and confirmed MPD communication (Fig. 5). During ERCP a plastic stent was placed for biliary drainage and jaundice resolution.
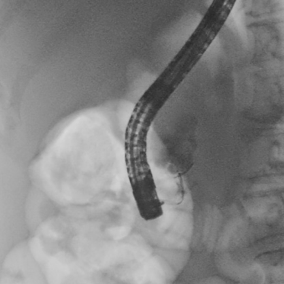
Figure 5. ERCP (pancreatography) : multicystic pancreatic head lesion with MPD communication.
Two months after, the patient underwent surgical resection of the pancreatic head lesion (Whipple procedure) and the final pathology confirmed the diagnosis of a serous cystadenoma of the pancreas.
Serous cystic neoplasms account for 8–17% of clinically encountered pancreatic cystic lesions and are predominantly found in middle-aged women (1). These lesions are usually benign and asymptomatic and present a benign clinical course in the vast majority of the patients (2). Symptoms may occur, typically in those patients with lesions > 4 cm in size, and are often attributed to mass effect or to infiltration of adjacent structures. Abdominal pain (25%), palpable mass (10%) and jaundice (7%) are the main clinical manifestations (3). Although rare, communication with the MPD has been reported occasionally (0- 0.6%) in serous cystic neoplasm, requiring a strong suspicion, so that the misdiagnosis of an intraductal papillary mucinous neoplasm is avoided (1).
REFERENCES
- Matsubayashi H, Oka Y, Ito T, et al. A Case of Serous Cystadenoma Communicating with a Stenotic Santorini’s Duct and Dilated Main Pancreatic Duct. J Gastrointestin Liver Dis. 2016 Dec;25(4):551-554.
-
Amico EC, Alves JR, de Araújo Lima Liguori A, et al. Serous Pancreatic Cystadenoma with Compression of Wirsung’s Duct. J Gastrointest Surg. 2019 Jan;23(1):176-178.
- Zhang XP, Yu ZX, Zhao YP, et al. Current perspectives on pancreatic serous cystic neoplasms: Diagnosis, management and beyond. World J Gastrointest Surg. 2016 Mar 27; 8(3): 202–211.
AUTHORS
Catarina Felix1; Susana Marques2; Joana Carmo1; Tiago Bana e Costa1; Miguel Bispo2; Mireia Castillo3; Cristina Chagas1
- Gastroenterology Department, Centro Hospitalar de Lisboa Ocidental, Lisbon, Portugal.
- Gastroenterology Department, Champalimaud Foundation, Lisbon, Portugal.
- Pathology Department, Champalimaud Foundation, Lisbon, Portugal.


