US Quiz of the Month – February 2022
CASE REPORT
A 44-year-old female patient presented in the last 8 months with non-productive cough and occasional right chest pain that worsened with lateral decubitus. Her past medical history was remarkable for uterine leiomyosarcoma that underwent surgery, chemotherapy and radiotherapy 8 years ago. She reported occupational exposure to acrylic compounds for 20 years and active smoking (about 2 pack-year for 4 years).
Thoraco-abdomino-pelvic CT revealed a large atypical lesion (82x68x46mm) in the left pulmonary lower lobe, central topography, with invasion of the posterior mediastinal fat and no cleavage plane with the esophagus, and small homolateral pulmonary hilar adenopathies. It was considered more likely to be a primary pulmonary lesion (Fig. 1).

Figure 1. Thoracic CT (axial view): atypical lesion in the left pulmonary lower lobe with invasion of the posterior mediastinal fat and no cleavage plane with the esophagus.
Subsequent bronchoscopy identified a bulging of the posterior segmental bronchus wall of the left lower lobar bronchus with normal-looking mucosa. Transbronchial needle aspiration, distal biopsies and bronchial brushing were performed but histopathological results were not conclusive.
The EUS evaluation identified, in topography concordant with station 8 of the mediastinum to the left of the aorta, a hypoechoic and heterogeneous lesion with well-defined limits measuring 40x44mm, without calcifications or vascular invasion, with loss of interface with the esophageal wall. Fine needle biopsy (FNB) using a 22G needle was performed (3 passes; 22G Acquire, Boston Scientific) obtaining material that was sent for histocytologic evaluation, nucleic acid amplification test for M. tuberculosis and microbiological examination (Fig. 2).
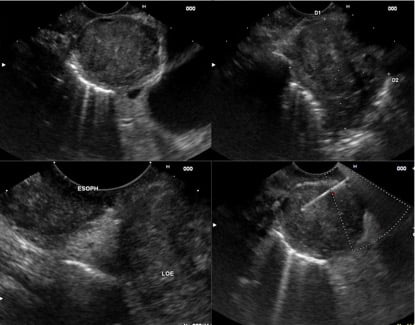
Figure 2. Linear EUS (transesophageal view): A and B – hypoechoic, heterogeneous, mediastinal lesion with well-defined limits measuring 40x44mm; C – loss of interface with the esophageal wall; D – FNB.
WHAT IS THE MOST LIKELY DIAGNOSIS?
DISCUSSION
Histocytological analysis identified a neoplasm composed of spindle cells with moderate to severe pleomorphism and hyperchromatic nuclei arranged in a fascicular pattern. The neoplastic cells were positive for smooth muscle actin (SMA) and desmin, and negative for S100 Protein, CKAE1/AE3, DOG1 and CD34 (Fig. 3).
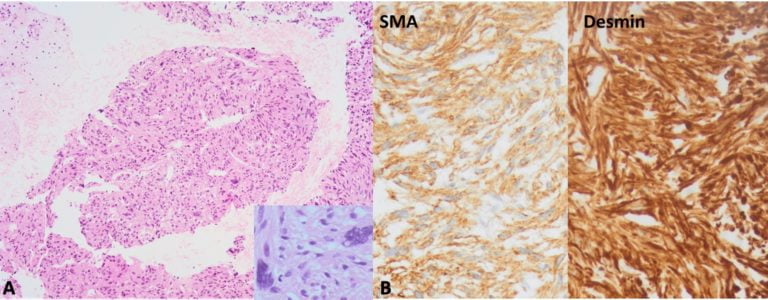
Figure 3. Pathology: A – Neoplasm composed of spindle cells with moderate to severe pleomorphism and hyperchromatic nuclei arranged in a fascicular pattern (Hematoxylin and eosin, magnification: 100x and 400x); B – Immunohistochemical staining positive for smooth muscle actin (SMA) and desmin (Magnification: 400x).
Although it was not possible to review the slides of the uterine tumor resected in 2013, based on the past medical history and actual pathological findings, the final diagnosis was uterine leiomyosarcomas (ULMS) metastasis. Staging cranioencephalic MRI also revealed an expansive intra-axial cortico-subcortical parasagittal occipital lesion on the right, with well-defined limits of approximately 25x23x21.5mm, suspected of metastasis. After discussion in a multidisciplinary meeting, the excision of the occipital lesion was decided. Anatomopathological examination of the surgical specimen revealed morphology and immunohistochemical profiles that were also compatible for leiomyosarcoma. Later, the patient started chemotherapy with Doxorubicin 60mg/m2 and Dacarbazine 750mg/m2, and is currently in the 4th cycle.
ULMS are rare conditions characterized by an aggressive behavior, with high rates of local recurrence and metastasis, leading to an early death (1). Usually metastasizes to the lungs and peritoneal cavity, followed by the retroperitoneum, liver and bone (2). The usual appearance of a lung metastasis is characterized by a large number of nodules, but the unilateral location of a mass does not rule out metastatic disease, as in this case (1). Lung metastasis often emerges soon after or even before the primary tumor is diagnosed. Nevertheless, they may develop after a long tumor-free interval, a fact that may complicate diagnosis (1). Clinical presentation may vary with symptoms as those seen in other primary lung neoplasms or they may be asymptomatic and found incidentally on imaging studies. (3) Because the metastatic neoplasms are much more common than the primary pulmonary leiomyosarcomas, all possible investigations should be undertaken to exclude the extrapulmonary primary origin (3). As suggested by this report, careful follow-up is recommended after ULMS treatment since metastatic leiomyosarcoma can relapse after a long period of time.
REFERENCES
- Carreiro, A., Frias, L., Miguel, A., Rocha, M., Carneiro, V., & Pavão, C. (2014). Unusual late lung metastasis from leiomyosarcoma of the uterus. Revista portuguesa de pneumologia, 20(4), 223-224.
- Guazzaroni, M., Tosti, D., Rascioni, M., Mataloni, M., Citraro, D., & Simonetti, G. (2014). Lung metastasis after an eighteen-years-long disease-free period since uterine leiomyosarcoma diagnosis. Case reports in oncological medicine, 2014.
- Nath, D., Arava, S., Joshi, P., Madan, K., & Mathur, S. (2015). Primary pulmonary leiomyosarcoma of lung: An unusual entity with brief review. Indian Journal of Pathology and Microbiology, 58(3), 338.
AUTHORS
Saraiva Ornelas R1, Pimentel J2, Santos S1, Carvalho D1, Ramos G1.
- Gastroenterology Department, Centro Hospitalar Universitário Lisboa Central, Portugal.
- Pathology Department, Centro Hospitalar Universitário Lisboa Central, Portugal.


