US Quiz of the Month – January 2020
CASE REPORT
A 65-year old asymptomatic male was referred to our Gastroenterology Department following incidental detection on abdominal ultrasound of a pancreatic head tumour, strongly hypoechoic, with 35mm in diameter, just above the confluence of the superior mesenteric and splenic veins. Magnetic resonance cholangiography (MRI) suggested a solid lesion measuring 30mm adjacent to the splenic-mesenteric-portal venous confluence and above the pancreatic isthmus; an identic lesion measuring 16mm was detected adjacent to the pancreatic tail (Fig. 1. and 2.).
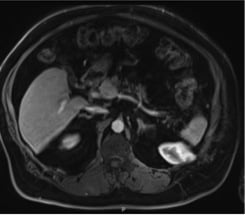
Figure 1. Abdominal and pelvic MRI (axial view): lesion adjacent to the splenic-mesenteric-portal venous confluence.

Figure 2. Abdominal and pelvic MRI (coronal view): lesion adjacent to the pancreatic tail.
Endoscopic ultrasonography (EUS) documented an anechoic structure with thin well-defined walls adjacent to the portal confluent and continuing with the splenic vein, 30mm in diameter, with positive colour Doppler and monophasic waveform in pulse wave Doppler study; this lesion was adjacent to the pancreas but with a clear interface with it (Fig. 3.). Adjacent to the pancreatic tail another lesion was identified, mildly hypoechoic, homogenous, well defined regular walls, 14mm in diameter, again with a clear interface with the pancreas and the spleen (Fig 4.).
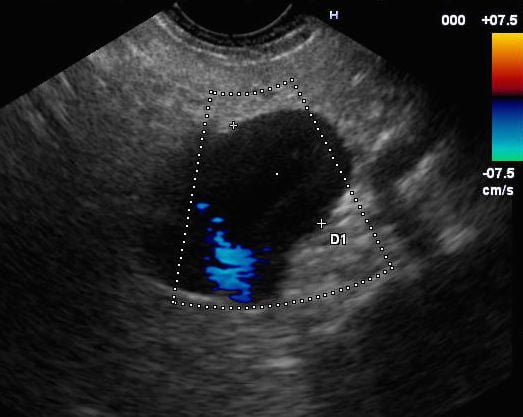
Figure 3. EUS: Anechoic structure adjacent to the portal confluent and continuing with the splenic vein, with positive colour Doppler and monophasic waveform.
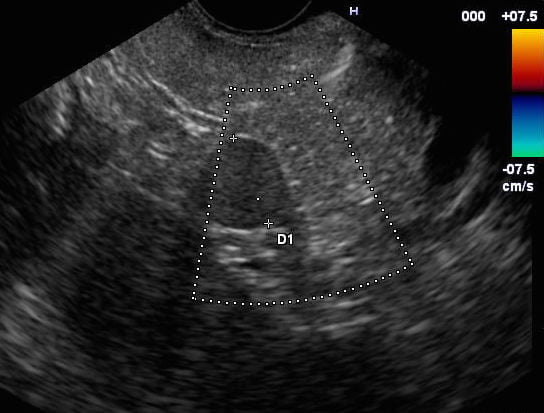
Figure 4. EUS: Hypoechoic lesion adjacent to the pancreatic tail.
WHAT IS THE MOST LIKELY DIAGNOSIS?
DISCUSSION
A wide range of anatomic variants and pathologic conditions in and around the pancreas may simulate primary pancreatic neoplasia at different imaging modalities. Based on EUS appearance of the lesion and its relation to the splenic vein, the diagnosis of splenic vein aneurysm was easily made. The smaller lesion had very different US characteristics suggesting an accessory spleen, due to its location and US features (namely similar echostructure to the adjacent spleen).
Venous system aneurysms are uncommon and splenic vein aneurysms are exceedingly rare. Lowenthal and Jacob described the first case of splenic vein aneurysm in 1953. Since then very few such cases have been reported. Congenital weakness of the venous wall, trauma, pancreatitis and portal hypertension are possible etiologies. They are usually asymptomatic and the diagnosis is generally made incidentally. However there is risk of aneurismal rupture, thrombosis, or local compressive effects. Because the incidence of these aneurysms is low, the exact indication for intervention and the type of treatment is not well defined. Most of the cases being asymptomatic are managed conservatively. Surgical intervention is recommended only in gradually enlarging and/or symptomatic splenic vein aneurysms.
An aneurysm of the splenic vein may mimic a pancreatic mass and result in unwanted surgery. EUS provides complementary details to computed tomography or magnetic resonance imaging in pancreatic and peri-pancreatic lesions, namely in vascular lesions. In the present case EUS made a correct diagnosis, thus an unnecessary surgery could be avoided.
REFERENCES
- To’o K, Raman S, Yu N, et al. Pancreatic and Peripancreatic Diseases Mimicking Primary Pancreatic Neoplasia. RadioGraphics. 2005;25(4), pp.949-965.
- Gupta A, Kumar Singhai M, Maheshwarappa R.P, et al. Splenic vein aneurysm: a rare clinical entity. Indian J Gastroenterol. 2013;32(3): 204-5.
- Heeren M, Op de Beeck B, Van den Brande P. Aneurysm of the splenic vein. Acta Chir Belg. 2004;104:322–4.
- Gharabaghi MA, Yazdi NA, Abrishami Z, et al. Splenic vein aneurysm. BMJ Case Rep. 2012; 2012:bcr1020115007.
AUTHORS
Verónica Pavão Borges1, Sara Santos1, Diana Carvalho1, Gonçalo Ramos1
- Gastroenterology Department, Centro Hospitalar Universitário de Lisboa Central, E.P.E


