US Quiz of the Month – July 2021
CASE REPORT
We present the case of a 65-year-old male patient with past medical history significant for mixed acinar-neuroendocrine carcinoma of the pancreas diagnosed in 2010, submitted to distal pancreatectomy and adjuvant chemotherapy, and multiple myeloma since 2020 (IgG kappa, ISS stage 1), under 2nd line chemotherapy, awaiting bone marrow transplantation. Due to an abnormal pancreatic head fluorodeoxyglucose (FDG) uptake (SUVmax 8.5) documented in PET-CT (Fig. 1), MRI was performed, which showed a 27x20mm hypovascular well delimited lesion in the pancreatic head (Fig. 2).
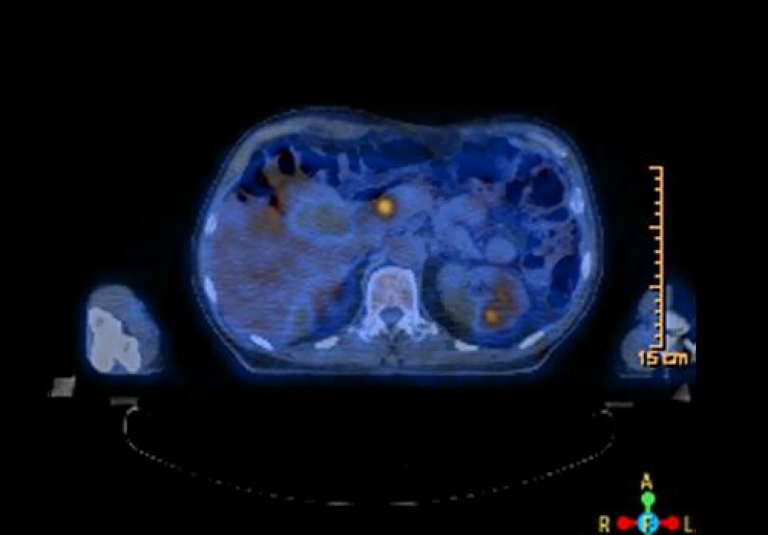
Figure 1. PET-CT FDG (axial view): abnormal FDG uptake in the pancreatic head.

Figure 2. Abdominal MR (axial view): 27x20mm hypovascular well delimited lesion in the pancreatic head.
Endoscopic ultrasound (EUS) confirmed a 27x25mm round homogeneous hypoechoic lesion, with well-defined contour, located in the pancreatic head, without upstream biliary or pancreatic duct dilation. An EUS-guided fine needle biopsy (EUS-FNB) of the lesion was performed using an Acquire 22G needle (2 passes) (Fig. 3).
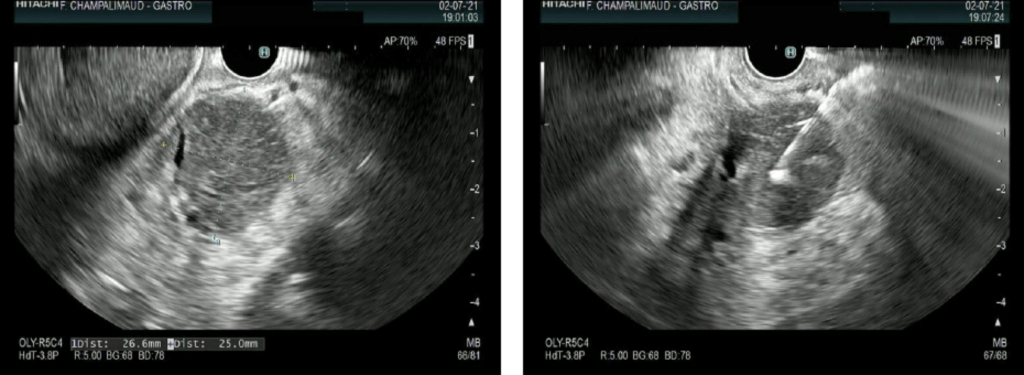
Figure 3. EUS (transduodenal): A) 27x25mm round homogeneous hypoechoic lesion, with well-defined contour, in the pancreatic head; B) EUS-FNB of the lesion.
WHAT IS THE MOST LIKELY DIAGNOSIS?
DISCUSSION
Pathology showed sheets of plasma cells (CK8/18-, Synaptophysin-, CD138+ and CD56+) with moderate cytologic atypia (Fig. 4), consistent with the diagnosis of extramedullary plasmocytoma involving the pancreas. The patient is now proposed for local radiotherapy of the pancreatic lesion and for 3rd line chemotherapy.
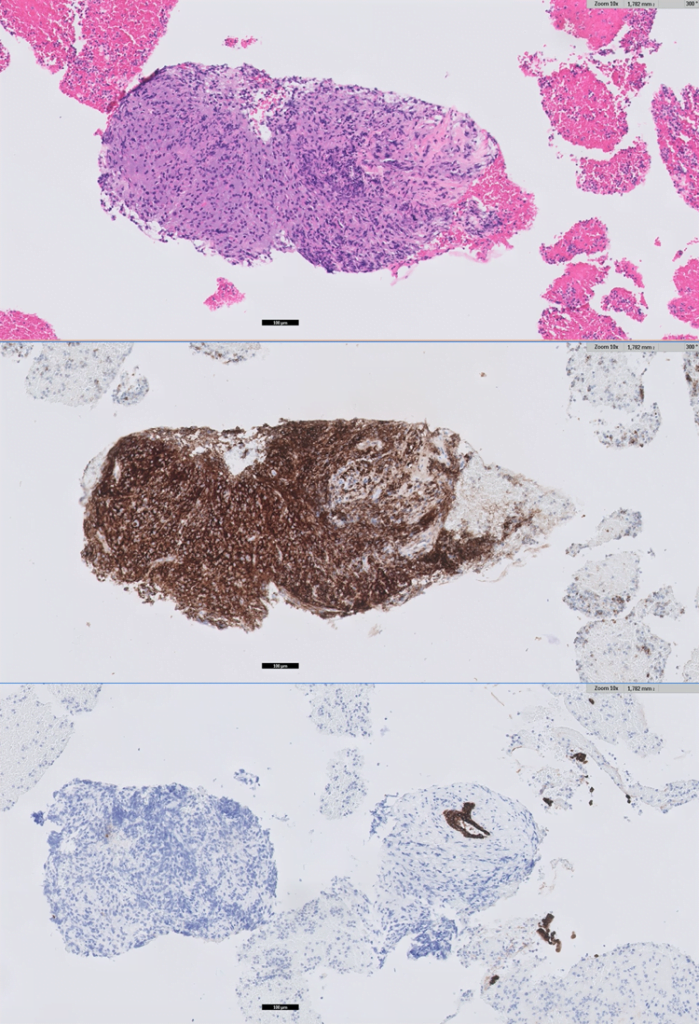
Figure 4. Pathology: sheets of plasma cells with moderate cytologic atypia, 10x – A) H&E, B) CK8/18-, C) CD138+.
Multiple myeloma (MM) is a plasma cell neoplasia and comprises 10-15% of all hematopoietic malignancies. MM may present as diffuse myelomatosis, as solitary myeloma of the bone or as an extramedullary plasmocytoma. Extramedullary plasmocytomas are uncommon, occurring in less than 5% of plasma cells neoplasms, and are usually associated with a more aggressive form of the disease. Though upper respiratory tract is the most common site for extramedullary involvement (80–90%), any tissue or organ, including the gastrointestinal tract (10%, mainly the liver), can be involved. Pancreatic involvement is extremely rare, with very few cases reported in the literature. The most common site of presentation is the pancreatic head and the most frequent clinical presentations are jaundice and abdominal pain. Although diffuse infiltration of the pancreas has been described in the literature, in the vast majority of the cases reported, as in our case, pancreatic plasmocytoma presented as a focal hypoechoic homogeneous mass with well-defined contour, which may be hypovascular on dynamic contrast-enhanced imaging. [1-3] These imaging findings impose a differential diagnosis with other solid pancreatic masses, especially with pancreatic neuroendocrine tumors (pNETs), which are characteristically hypervascular. [4] Therefore, a pathologic diagnosis using EUS-guided tissue acquisition is crucial for an accurate diagnosis. A correct diagnosis obviates unnecessary surgery, as this neoplasm responds well to local radiotherapy. [1]
In conclusion, in a patient with MM presenting with a pancreatic mass, the diagnosis of pancreatic plasmocytoma must be considered and EUS-guided tissue acquisition should be performed to ensure the correct diagnosis and management of the patient.
REFERENCES
- Hiller N, Goitein O, Ashkenazi YJ. Plasmacytoma of the pancreas. Isr Med Assoc J. 2004 Nov;6(11):704-5.
- Hatem M, So B, Gray R, Wong J. Plasmocytoma presented as pancreatic head mass. Radiol Case Rep. 2015 Aug 28;10(4):81-7.
- de Sousa CSM, de Miranda CLVM, Avelino MC, Bastos BB, Mendes ILL. Diffuse plasmacytoma of the pancreas: a rare entity. Radiol Bras. 2017 Sep-Oct;50(5):344-345.
- Lu T, Pu H, Zhao G. Primary pancreatic plasmacytoma: a rare case report. BMC Gastroenterol. 2017 Dec 20;17(1):167.
AUTHORS
Susana Marques1, Miguel Bispo1, Sara Teles Campos1, Ricardo Rio-Tinto1, Paulo Fidalgo1, Antonio Galzerano2, Jacques Devière1,3
- Department of Gastroenterology and Digestive Endoscopy, Digestive Unit, Champalimaud Foundation, Lisbon, Portugal
- Department of Pathology, Digestive Unit, Champalimaud Foundation, Lisbon, Portugal
- Department of Gastroenterology, Hepatopancreatology, and Digestive Oncology, Erasme University Hospital – Université Libre de Bruxelles, Brussels, Belgium


