US Quiz of the Month – June 2020
CASE REPORT
A 75-year-old male with abdominal pain was admitted to our hospital. Physical examination revealed painful left hypochondrium with a palpable spleen. Blood tests revealed anemia (11 g/dL), normal white cell count (9710 uL) with high lymphocyte ratio (66,5%), thrombocytopenia (101000 uL), elevated β2-microglobulin (7,82 mg/L), monoclonal hypergammaglobulinemia (0,52 g/dL) and urinary Bence Jones λ proteinuria. The blood smear showed atypical lymphocytes and imunnophenotyping revealed B lymphocytes with restriction for superficial light λ chains, CD45+, CD19+, CD20+, CD23-, CD5-, CD10-, CD200-, CD79b+(weak), CD43-. Abdominal ultrasound noted an enlarged spleen and a 5cm solid lesion in the gastric body. Computed tomography (CT) scan was performed and showed abdominal lymphadenopaphies, the largest with 12 mm, and the already known gastric lesion with contrast enhancement (Fig. 1).
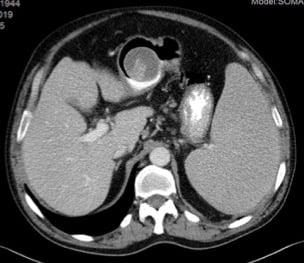
Figure 1. Contrast enhanced CT (axial view): solid lesion located in the body of the stomach.
At this moment, it was important to clarify whether the gastric lesion was related to the known lymphoma or if indeed another diagnosis was present that could change clinical management. Therefore, upper gastrointestinal was performed and revealed a subepitelial lesion (Fig. 2).
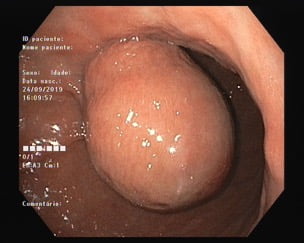
Figure 2. Upper endoscopy: subepithelial lesion located in the gastric body.
Further characterization of this lesion by yndoscopic ultrasound (Olympus curvilinear GF-UCT 180 ultrassound gastrovideoscope; Aloka prosound α10) confirmed a 45mm subepithelial lesion in the gastric body, within the third lawyer of the gastric wall (submucosa). The lesion appearance was heterogeneous, being predominantly anechoic, but revealing a solid component that was Doppler positive (Fig. 3).

Figure 3. EUS (transgastric): heterogenous subepithelial lesion located in the gastric body, showing a doppler positive solid component.
EUS-FNA using a 22G needle was performed aiming at the solid component. Four cc of dark haematic fluid were collected and small intralesional bleeding was witnessed without clinical impact. Intravenous quinolone was administered. Multiple suspicious celiac lymph nodes were identified and EUS-FNA of one of them using a 25G needle was also performed. Rapid on-site evaluation (ROSE) was available, so all the samples were assessed by the pathologist and proceeded for cytoblock as well as for flow cytometry.
WHAT IS THE MOST LIKELY DIAGNOSIS?
DISCUSSION
Results from EUS-FNA and flow cytometry showed numerous small monomorphic lymphocytes (Fig. 4) consistent with diffuse small B-cell lymphoma (non-Hodgkin B lymphoma CD5-, CD10- by flow cytometry).

Figure 4. Cytology (H&E, x40): numerous small monomorphic lymphocytes.
Gastric subepithelial lesions can be benign or malignant and EUS-FNA should be performed when results are likely to change patient management decisions.1 The prevalence of gastrointestinal subepithelial tumor has been reported to be 0.36%– 1.94%. 2 Secondary GI involvement by lymphoma is far more common than primary GI lymphoma, the latter accounting for about 15%–20% of GI lymphomas. The stomach is most commonly involved and diffuse large B cell lymphomas are the most common subtype.3,4
In this case it was important to know if there was a disease affecting the gastric wall and possibly regional lymph nodes other than the lymphoma already diagnosed by peripheral blood analysis and EUS-FNA was mandatory to clarify this.5 If so, the therapeutic plan could have been altered. Our lesion revealed to be the same type of lymphoma as the one discovered in the initial blood investigation.
The richness of this clinical case is the rarity of the EUS images because it is unusual for lymphoma to present as subepithelial lesion. Adding to the rarity of the case, the lesion was heterogeneous, being mostly anechoic within the submucosa layer, but showing a solid component. This appearance contrasts with the usual lymphoma appearance as homogeneous hypoechoic lesions located between the second and fourth layers with layer disruption.6 Furthermore, it is to our best knowledge the only EUS image of gastric lymphoma as a subepithelial lesion where an anechoic cavity within submucosa layer showed a clear solid component within.
REFERENCES
- Hawes, R., Fockens, P. & Varadarajulu, S. (2019). Endosonography 4 edition. Philadelphia, PA: Elsevier.
- Kim S, Song J, Hwang J. Current Status of Endoscopic Ultrasonography in Gastrointestinal Subepithelial Tumors. Clin Endosc. 2019;52(4):301-305.
- Fleming JP , Smith K , Bennett R , et al.A case of primary gastrointestinal lymphoma presenting as colonic perforation. J Case Rep Images Surg 2017;3:29–34.
- Koch P , del Valle F , Berdel WE , et al. Primary gastrointestinal non-Hodgkin’s lymphoma: II. Combined surgical and conservative or conservative management only in localized gastric lymphoma–results of the prospective German Multicenter Study GIT NHL 01/92. J Clin Oncol 2001;19:3874–83.
- Zucca E, Copie-Bergman C, Ricardi U, Thieblemont C, Raderer M, Ladetto M. Gastric marginal zone lymphoma of MALT type: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Annals of Oncology. 2013;24(suppl 6):vi144-vi148.
- Gong EJ, Kim DH. Endoscopic Ultrasonography in the Diagnosis of Gastric Subepithelial Lesions. Clin Endosc. 2016;49(5):425–433.
AUTHORS
António Oliveira1, Rui Loureiro1, Helena Oliveira2, Catarina Fidalgo1.
- Gastroenterology Department, Hospital Beatriz Ângelo, Loures, Portugal
- Pathology Department, Hospital Beatriz Ângelo, Loures, Portugal


