US Quiz of the Month – May 2021
CASE REPORT
We present the case of a 56-year-old man with past medical history significant for asymptomatic gallstones. Due to intermediate probability of choledocholithiasis, an MRCP was performed and showed a scleroatrophic gallbladder with stones, no choledocolithiasis and an unspecific 8-mm area with signal changes in the perfusion images located in the pancreatic body. To further characterize the pancreatic incidental finding, the patient was referred to our institution and an EUS was done and found in the distal pancreatic body 4 hypoechoic homogeneous round lesions, between 4 to 7mm in size, with well-defined contour (Video 1). EUS-guided FNB of the 2 largest lesions was performed using an Acquire 22-gauge needle (3 passes in total).
WHAT IS THE MOST LIKELY DIAGNOSIS?
DISCUSSION
In patients with multiple pancreatic lesions with the previously mentioned US characteristics (hypoechoic homogeneous round lesions, with well-defined contour) the most commonly found diagnosis is multifocal pNET. However, and interestingly, this was not the case with regard to this patient as pathology revealed lymphoid tissue in both cases, with groups of CD45 positive and CK8/18 negative cells, supporting the diagnosis of intrapancreatic accessory spleens (Figure 1). To our knowledge, this is the first case of multiple intrapancreatic accessory spleens documented by EUS in the literature.
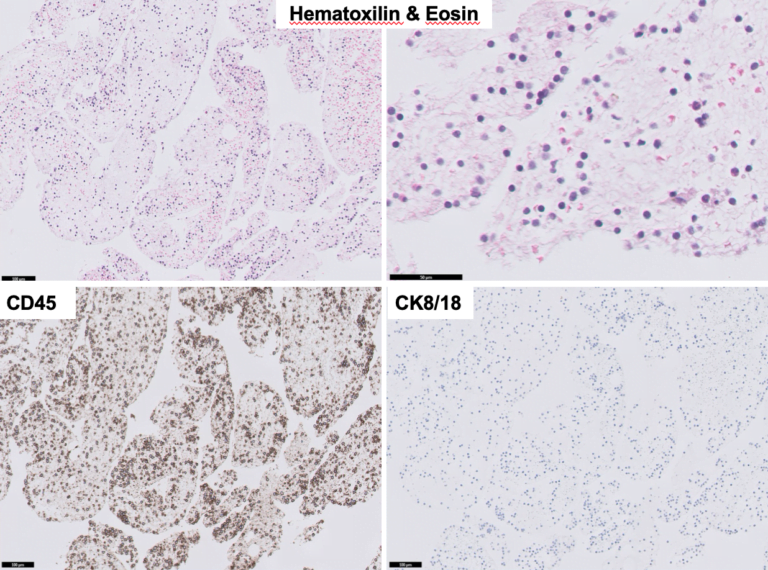
Figure 1. Pathology (EUS-guided FNB): lymphoid tissue, with groups of CD45 positive and CK8/18 negative cells.
Accessory spleen is a common benign congenital anomaly, with an approximate prevalence of 10–30% [1]. The most frequent location is the splenic hilum (80%), followed by the pancreatic tail (17%) [2]. Intrapancreatic accessory spleen (IPAS) is usually diagnosed incidentally on abdominal US, computed tomography, or magnetic resonance imaging. Usually, it is a single hypervascular lesion in the pancreatic tail, with imaging characteristics similar to the adjacent spleen [3]. However, as a well-defined homogeneous and hypervascular lesion, it is most frequently misdiagnosed as pancreatic NET. Consequently, many patients undergo an unnecessary pancreatic resection. In this situation, EUS can be very useful to achieve a diagnosis. Endosonographically, intrapancreatic accessory spleen is a round-to-oval-shaped, small lesion, usually less than 2cm, with well-defined margins, a homogeneous echotexture, and an echogenicity lower than the adjacent pancreas and identical to that of the spleen. EUS Doppler mode may confirm its increased vascularity [1, 4]. As a hypervascular pancreatic lesion, using contrast-enhanced EUS, intrapancreatic accessory spleen typically shows a marked and homogeneous hyperenhancing appearance during the arterial phase compared with the surrounding pancreatic parenchyma [4, 5]. EUS-FNA/B can also be performed and is safe and effective, confirming the diagnosis in 90% of the cases and with no complications reported [6].
In conclusion, when an asymptomatic pancreatic mass is detected, the diagnosis of intrapancreatic accessory spleen should be kept in mind, especially if the lesion has the same imaging features as the spleen. Because it is crucial to accurately differentiate intrapancreatic accessory spleen from pNETs, EUS-FNA/B should be performed to ensure the correct diagnosis and management.
REFERENCES
- Krishna SG, Heif MM, Sharma SG, Pandey T, Rego RF. Intrapancreatic accessory spleen: investigative dilemmas and role of EUS-guided FNA for diagnostic confirmation. JOP. 2011;12:603–606.
- Halpert B, Gyorkey F. Lesions observed in accessory spleens of 3,011 patients. Am J Clin Pathol. 1959;32:165–168.
- Okun SD, Lewin DN. Non-neoplastic pancreatic lesions that may mimic malignancy. Semin Diagn Pathol. 2015;33:31–42.
- De Robertis R, D’Onofio M, Manfrin E, et al. A rare case of pancreatic head splenosis diagnosed by contrast-enhanced ultrasound. Ultraschall Med. 2014;35:72–74.
- Will U, Arciadacono P, Petrone MC, et al. Differential diagnosis of small solid pancreatic lesions. Gastrointest Endosc. 2016;84:933–940.
- Ardengh C, Lopes V, Kemp R, Lima-Filho ER, Venco F. Pancreatic splenosis mimicking neuroendocrine tumors: endoscopic ultrasound guided fine needle aspiration. Arq Gastroenterol. 2013;50:10–14.
AUTHORS
Susana Marques1, Miguel Bispo1, Sara Teles Campos1, Ricardo Rio-Tinto1, Paulo Fidalgo1, Mireia Castillo-Martin2, Jacques Devière1,3
- Department of Gastroenterology and Digestive Endoscopy, Digestive Unit, Champalimaud Foundation, Lisbon, Portugal
- Department of Pathology, Digestive Unit, Champalimaud Foundation, Lisbon, Portugal
- Department of Gastroenterology, Hepatopancreatology, and Digestive Oncology, Erasme University Hospital – Université Libre de Bruxelles, Brussels, Belgium


