US Quiz of the Month – October 2021
CASE REPORT
The authors present the case of an 81-year-old male patient with a history of smoking and hypertension, referred for an endoscopic ultrasound (EUS) due to the appearance of obstructive jaundice. The patient previously performed abdominal CT scan that revealed a pancreatic head mass, measuring 40x40mm and multiple bone lesions in the sternum and ribs. Laboratory study revealed hyperbilirubinemia (total bilirubin 4.3 mg/dL, direct bilirubin 3.2 mg/dL) and cholestasis (alkaline phosphatase 341U/I, gamma-glutamyl transferase 641 U/I). CA 19.9 and carcinoembryonic antigen were normal. EUS revealed in the cephalopancreatic region a vaguely nodular area, heterogeneous, hypoechogenic, and with ill-defined limits and contours, with approximately 36x37mm (Figure 1). The elastography study of the lesion revealed a heterogeneous green pattern with a strain-ratio of 6.8 (Figure 2). The main pancreatic duct had a normal caliber in the body and tail, with mild ectasia in the cephalic/periampullary region. Tissue sampling was obtained through fine needle biopsy (FNB), 2 passages, using an AcquireTM 22G needle (Boston Scientific).
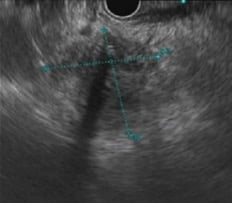
Figure 1. EUS (transduodenal view): nodular lesion, heterogeneous, hypoechogenic, and with ill-defined limits in the cephalopancreatic region.
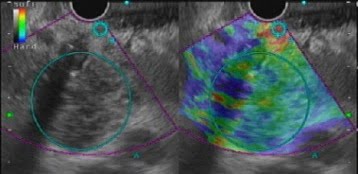
Figure 2: EUS (transduodenal view): elastography study of the lesion revealed a heterogeneous green pattern with a strain-ratio of 6.8.
Histopathological analysis identified an infiltration of the pancreatic parenchyma with intermediate size anaplastic cells, some of which with plasmacytoid phenotype. Immunohistologically there was positivity of CD138; proliferative activity assessed by Ki67 was 80%, and CD20 and cytokeratins were negative.
WHAT IS THE MOST LIKELY DIAGNOSIS?
DISCUSSION
The histopathological analysis was compatible with a pancreatic plasmacytoma.
About 5% of plasma cell tumors form an isolated solitary lesion, called plasmacytoma.1 Extramedullary plasmacytoma is a very rare tumor derived from plasma cells and found outside the bone marrow.
Only 10% of extramedullary plasmacytomas occur in the gastrointestinal tract, where they are detected most often in the stomach.2 Rarely, the pancreas is infiltrated by plasmacytes, being found in approximately 2.3% of autopsies. Although plasmacytoma can develop in any part of the pancreas; the most frequent site of the tumor is the pancreatic head. 2
Common signs and symptoms in patients with pancreatic plasmacytoma included abdominal pain, obstructive jaundice, and anorexia.
EUS usually shows a hypoechoic, heterogeneous and well defined mass in relation to the normal pancreatic echotexture. EUS with FNB is a fast and reliable technique for diagnosis and should be the first choice for tissue evaluation.3
Histology shown atypical plasma cells, which are positively immunostained for CD138, and the k light chain are helpful for differential diagnosis in a case with pancreatic mass.4
Treatment options include surgery, radiotherapy, chemotherapy, and combinations of them. The course is more favorable in cases with primary plasmacytoma than that of that of plasmacytoma accompanying multiple myeloma.
REFERENCES
- Dores GM, Landgren O, McGlynn KA, Curtis RE, Linet MS, Devesa SS. Plasmacytoma of bone, extramedullary plasmacytoma, and multiple myeloma: incidence and survival in the United States, 1992-2004. Br J Haematol. 2009;144(1):86-94.
- Lu, T., Pu, H., Zhao, G. Primary pancreatic plasmacytoma: a rare case report. BMC Gastroenterol. 2017;17:67.
- Williet N, Kassir R, Cuilleron M, et al. Difficult endoscopic diagnosis of a pancreatic plasmacytoma: Case report and review of literature. World J Clin Oncol. 2017;8(1):91-95.
- Lopes de Silva R. Pancreatic involvement by plasma cell neoplasms. J Gastrointest Cancer. 2012;43(2):157-61.
AUTHORS
Dorelo R1, Ferreira-Silva J2, Vilas-Boas F2, Macedo G2.
- World Gastroenterology Organization Porto Training Center, Centro Hospitalar Universitário de São João, Portugal
- Gastroenterology Department, Centro Hospitalar Universitário de São João, Portugal


