US Quiz of the Month – September 2021
CASE REPORT
The authors present the case of a 73-year-old male patient with a history of smoking and chronic obstructive pulmonary disease. A thoracic CT scan was performed and revealed multiple esophageal nodules in all segments (Fig. 1).

Figure 1. Thoracic CT scan, coronal and sagittal views: Multiple nodules are observed along the esophageal wall (arrows).
The patient was asymptomatic, with no dysphagia, thoracic or epigastric pain or weight loss. An esophagogastroscopy was performed and documented multiple bulges covered by normal mucosa, non-pulsatile, of hard consistency without pillow sign (Fig. 2).

Figure 2. Esophagogastroscopy: Multiple bulges covered by normal mucosa, non-pulsatile, of hard consistency without pillow sign.
Endoscopic ultrasonography (EUS) revealed hypoechoic nodules arising from the fourth layer of the esophageal wall, the largest with 25×18 mm (Fig. 3). Fine needle biopsies (FNB) were performed (Acquire 22 G, Boston Scientific).
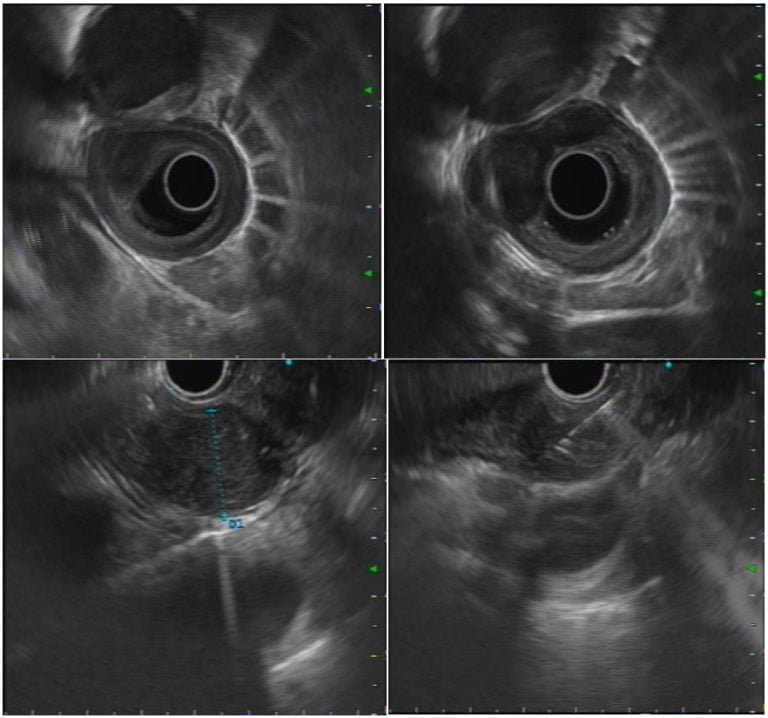
Figure 3. EUS: Hypoechoic nodules arising from the fourth layer of the esophageal wall, the largest with 25×18 mm; FNB were performed.
WHAT IS THE MOST LIKELY DIAGNOSIS?
DISCUSSION
These findings were compatible with multiple leiomyomas. Histopathological analysis revealed benign leiomyomatous cellular proliferation, positive for muscle specific actin and negative for CD117 and S100. A final diagnosis of multiple leiomyomas was made.
Primary intramural benign tumors of the esophagus are responsible for 2% of all esophageal tumors [1]. Leiomyoma is the most common solid benign tumor of the esophagus, and comprises of around 70% of esophageal subepithelial lesions [2,3]. It occurs more often in male patients (2:1) at a median age of 30-35 years and rarely presents as multiple lesions, with few cases reported [1]. By EUS, leiomyomas present as well-defined hypoechoic nodules in the muscularis propria or the muscularis mucosae (fourth and second EUS layers, respectively) [4]. Histology demonstrates well-differentiated smooth muscle cells with immunohistochemical findings positive for muscle actin and negative for CD117 and S100. CD117 corresponds to c-Kit protein activation and is a sensitive marker for gastrointestinal stromal tumors and S100 is a marker of granular cell tumors [4].
The presence of multiple leiomyomas is distinguished from esophageal leiomyomatosis, an extremely rare benign pseudomuscular hypertrophy of the esophageal wall associated in most male cases with the X-linked Alport syndrome [5]. In the present case there are discrete tumor nodules in the muscularis propria rather than a diffuse hypertrophy of the muscular layer and there is no history of chronic kidney disease despite the old age of the patient nor other signs and symptoms of Alport syndrome.
Considering that the risk of malignant transformation is low [4,6] and the patient was asymptomatic, a conservative approach was adopted. The development of symptoms, particularly dysphagia, or evidence of nodule growth demands further investigation and possibly an intervention.
REFERENCES
- Djakovic Z, Stancic-Rokotov D, Djakovic I. Multiple esophageal leiomyomas: case report, Acta Chirurgica Croatica. 2020;17:35-36.
- Baysal B, Masri OA, Eloubeidi MA, Hakan S. The role of EUS and EUS-guided FNA in the management of subepithelial lesions of the esophagus: A large, single-center experience. Endoscopic Ultrasound. 2017;6(5):308-316.
- Yang PS, Kyung SL, Soon JL, et al. Esophageal Leiomyoma: Radiologic Findings in 12 Patients. Korean Journal of Radiology. 2001;2(3):132-137.
- Al-Lehibi A, Bamakhrama K. Role of Endoscopics Ultrasound in Subepithelial Lesions (SELs) Chapter 2. In: Chong C. Endoscopic Ultrasound – From Usual to Special. China: Chinese University of Hong Kong, 2017. p. 13-32.
- Prenzel KL, Schäfer E, Stippel D, et al. Multiple giant leiomyomas of the esophagus and stomach. Diseases of the Esophagus. 2006; 19:504-508.
- Codipilly DC, Fang H, Alexander JA, et al. Subepithelial esophageal tumors: a single-center review of resected and surveilled lesions. Gastrointestinal Endoscopy. 2018; 87(2):370-377.
AUTHORS
Diogo Bernardo Moura1, Nuno Nunes1, Margarida Flor de Lima1, Carolina Chálim Rebelo1, Maria Antónia Duarte1.
- Gastroenterology Department, Hospital do Divino Espírito Santo de Ponta Delgada, Ponta Delgada, Portugal.


