US Quiz of the Month – junho 2025
Case Report
A 36-year-old female with no significant medical history and no known drug allergies was referred to the Gastroenterology Department following the incidental detection of a gastric subepithelial lesion during an upper endoscopy. The patient reported epigastric discomfort, which had prompted the initial endoscopic evaluation. She denied other gastrointestinal symptoms or unintentional weight loss. Physical examination was unremarkable.
Endoscopic ultrasound (EUS) demonstrated a heterogeneous, predominantly hypoechoic lesion with extensive internal calcification, originating from the muscularis propria (Figure 1). EUS-guided fine needle biopsy (FNB) was performed, but histological examination was inconclusive, revealing fibromuscular tissue and focal mature adipocytes.
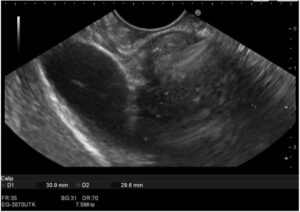
Figure 1: EUS image showing a heterogeneous calcified lesion.
Contrast-enhanced computed tomography revealed a well-defined, 30 × 30mm nodular lesion with dense internal calcification arising from the gastric antrum wall, without unequivocal arterial phase contrast enhancement (Figure 2).
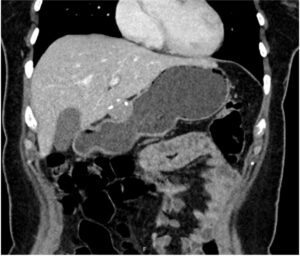
Figure 2: Contrast-enhanced CT scan showing a gastric wall nodular lesion with peripheral calcifications.
Due to diagnostic uncertainty, the patient underwent two additional EUS procedures between December 2023 and April 2024. Despite fine-needle aspiration and FNB using 22G and 25G needles, with adequate tissue sampling judged by macroscopic on-site evaluation, histology was ultimately non-diagnostic. Due to persistent diagnostic ambiguity, with no possibility to preoperatively exclude GIST, the case was discussed in a multidisciplinary meeting, and the patient underwent an atypical gastrectomy in October 2024.
Histopathological analysis revealed a well-circumscribed, sclerotic tumor with extensive calcification, composed of bland spindle cells embedded in dense collagen and a lymphoplasmacytic inflammatory infiltrate (Figure 3).
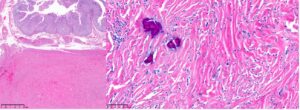
Figure 3: Calcifying fibrous tumor of the stomach. Histological section showing a well-circumscribed lesion centered in the muscularis propria (Left, HE, 10x), composed of bland spindle cells embedded in hyalinized stroma, with scattered calcifications and a lymphoplasmacytic infiltrate (Right, HE, 200x).
The tumor had a low mitotic index and there was no evidence of necrosis or vascular invasion. Immunohistochemical staining was negative for smooth muscle actin (SMA), DOG1, c-Kit, CD34, S100, and ALK. Stromal plasma cells expressed CD38 without IgG4 positivity.
What is the most likely diagnosis in a gastric subepithelial lesion with extensive calcification, bland spindle cells, and negative immunostaining for SMA, c-Kit, DOG1, S100, and CD34?
Discussion
Gastric subepithelial lesions often present a diagnostic challenge, particularly when standard biopsy techniques yield limited or inconclusive results (1). In our case, the lesion’s extensive calcification significantly impaired EUS visualization/characterization and tissue acquisition, leading to repeated non-diagnostic preoperative sampling. Ultimately, surgical resection was required to establish a definitive diagnosis.
Calcifying fibrous tumor (CFT) is a rare, benign mesenchymal neoplasm that typically arises in adults, with a slight female predominance (2). It is often discovered incidentally or presents with nonspecific symptoms, such as abdominal discomfort. The stomach, particularly the gastric antrum, is one of the most common sites of gastrointestinal involvement.
Despite its benign nature, CFT can closely mimic (pre)malignant subepithelial tumors on imaging and endoscopy due to its hypoechoic echotexture and frequent calcifications. These features often raise suspicion for gastrointestinal stromal tumors, leading to diagnostic uncertainty and potential overtreatment. Immunohistochemistry is crucial for accurate diagnosis, as CFT demonstrates a distinctive immunophenotypic profile.
Recurrence is rare after surgical resection. Therefore, awareness of the imaging, histological, and immunohistochemical features of CFT is crucial to ensure correct diagnosis and avoid unnecessary overtreatment.
References
- Vasilakis T, Ziogas D, Tziatzios G, Gkolfakis P, Koukoulioti E, Kapizioni C, et al. EUS-Guided Diagnosis of Gastric Subepithelial Lesions, What Is New? Diagnostics (Basel). 2023;13(13).
- Turbiville D, Zhang X. Calcifying fibrous tumor of the gastrointestinal tract: A clinicopathologic review and update. World J Gastroenterol. 2020;26(37):5597-605.
Authors
Joana Mota1,2, João Carlos Almeida2,3, Filipe Vilas Boas1,2, Eduardo Rodrigues Pinto1,2, Guilherme Macedo1,2
1 Gastroenterology Department, Centro Hospitalar Universitário São João, Porto, Portugal.
2 Faculty of Medicine of the University of Porto, Porto, Portugal.
3 Pathology Department, Centro Hospitalar Universitário São João, Porto, Portugal


