US Quiz of the Month – Agosto 2022
CASE REPORT
The authors present the case of a 65-year-old male patient, smoker, with history of hypertension, Paget’s disease, Gilbert syndrome and right nephrectomy 20 years ago due to renal cell carcinoma. He presented to consultation with complains of abdominal pain and weight loss. Upon investigation, abdominopelvic computer tomography revealed multiple bilateral pulmonary nodules, a pericentimetric nodule in the pancreatic neck and a 25mm adrenal nodule and mediastinal adenopathies (Figure 1). After multidisciplinary discussion, pancreatic biopsy was proposed.
Endoscopic ultrasound (EUS) showed a 13mm well-defined hypoechogenic pancreatic nodule, located in the pancreatic neck (Figure 2), predominantly green on elastography (strain ratio 2.2). A 22-gauge fine needle biopsy was performed. Pathology showed pancreatic parenchyma with necrosis and infiltration by atypical clear monomorphonuclear cells with bright cytoplasm. Imunohistochemistry was positive for PAX8 and negative for trypsin, synaptophysin and chromogranin (Figure 3).

Figure 1: Abdominopelvic computer tomography revealing a pericentimetric nodule in pancreatic neck (red arrow) and a 25mm adrenal nodule (green arrow).
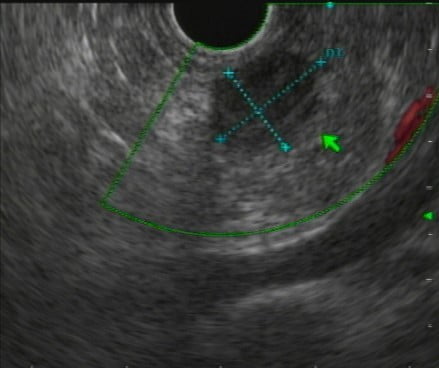
Figure 2: Endoscopic ultrasound (EUS) showed a 13mm well-defined hypoechogenic pancreatic nodule, located in pancreatic neck.
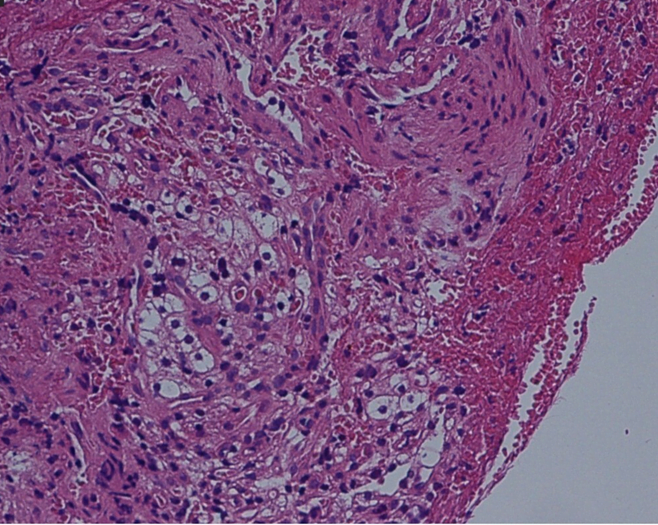
Figure 3: Pathology specimen shows atypical clear monomorphonuclear cells with bright cytoplasm.
QUIZ - WHAT IS THE MOST LIKELY DIAGNOSIS?
DISCUSSION
These findings were compatible with pancreatic metastasis of renal cell carcinoma and the patient initiated sunitinib
The frequency of pancreatic metastases ranges between 2% and 5% of all pancreatic malignant tumors [1]. However, the pancreas is an elective site for metastases from renal cell carcinoma (RCC). In many cases, it can be difficult to distinguish a pancreatic RCC metastasis from a primary pancreatic ductal adenocarcinoma (PDAC) or a neuroendocrine tumor (NET) of the pancreas. Patients are often asymptomatic, but may develop symptoms of epigastric abdominal pain or acute pancreatitis secondary to pancreatic ductal obstruction [2].
RCC metastatic disease to the pancreas can often be distinguished from PDAC with cross-sectional images, as the former lesion is hypervascular while the latter lesion typically appears hypointense in the contrast phase [2]. Metastases to the pancreas can be multicentric and typically do not cause peripancreatic lymphadenopathy. Pancreatic NETs are also hypervascular and distinguishing it from RCC metastases to the pancreas can be difficult [3].
Most cases of RCC metastasis to the pancreas present as metachronous lesions, often many years after resection of the primary tumor [4]. The average time to presentation for pancreatic metastasis from RCC is 9 years after the initial resection [5]. This finding highlights the importance of long-term post-nephrectomy surveillance in patients with RCC. Although metastasis to the pancreas is most commonly associated with disseminated systemic disease, an isolated pancreatic lesion may be amenable to surgical treatment.
REFERENCES
- Ballarin R, Spaggiari M, Cautero N et al. Pancreatic metastases from renal cell carcinoma: the state of the art. World J Gastroenterol 2011; 17: 4747-4756. doi:10.3748/wjg.v17.i43.4747
- Lavu H, Yeo CJ. Metastatic renal cell carcinoma to the pancreas. Gastroenterol Hepatol (N Y) 2011; 7: 699-700.
- Minni F, Casadei R, Perenze B et al. Pancreatic metastases: observations of three cases and review of the literature. Pancreatology 2004; 4: 509-520. doi:10.1159/000080248
- Sohn TA, Yeo CJ, Cameron JL et al. Renal cell carcinoma metastatic to the pancreas: results of surgical management. J Gastrointest Surg 2001; 5: 346-351. doi:10.1016/s1091-255x(01)80060-3
- Golimbu M, Al-Askari S, Tessler A et al. Aggressive treatment of metastatic renal cancer. J Urol 1986; 136: 805-807. doi:10.1016/s0022-5347(17)45085-3
AUTHORS
Ferreira-Silva J1, Medas R1, Moutinho-Ribeiro P1, Macedo G1
1 – Gastroenterology Department, Centro Hospitalar Universitário de São João, Portugal


