US Quiz of the Month – Dezembro 2022
CASE REPORT
We present a case of a 67-year-old male patient with a past medical history of severe acute biliary pancreatitis complicated by pancreatic necrosis and pseudocyst. A pancreatic pseudocyst drainage at the time, 3 years before, was performed guided by endoscopic ultrasound (EUS). The patient resorted to the emergency room (ER) because of abdominal pain located in the epigastrium that was exacerbated with food and was associated with vomiting. Additionally, the patient had fever and 3-4 diarrheal stools without blood or mucus. Laboratory analysis revealed a C-reactive protein of 375 mg/L, without leucocytosis.
The computed tomography (CT) (Fig. 1) in the ER revealed the presence of hypodense nodular lesions, with the two largest located in the right hepatic lobe and reaching about 70mm and 75 mm in maximum diameter. There were no signs of acute pancreatitis, and the pseudocyst was resolved.

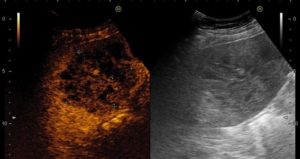
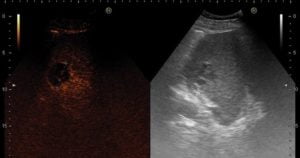
Fig. 1 – Computed tomography images showing the two largest hypodense nodular lesions in the right hepatic lobe (A-B).
Conventional ultrasound revealed heterogeneity of the hepatic parenchyma caused by poorly defined various slightly hypoechoic and isoechoic inhomogeneous focal lesions (Fig. 2 A).


Fig. 2 – A. Conventional B-mode ultrasound showing two hypoechoic inhomogeneous lesions. CEUS images showing: B. one nodular lesion in segment V/VIII with honeycomb appearance in the arterial phase; C. one smaller nodular lesion in segment VII with rim enhancement in the venous phase.
Contrast-enhanced ultrasound (CEUS) was made. The two largest lesions in the right hepatic lobe were observed during the 3 venous phases after endovenous contrast injection (Sonovue© 2,4mL), 1 in segment V/VIII with 80 mm and 1 in the segment VI with 70 mm, presenting in the arterial phase a peripheral and very dense septa enhancement, giving them a honeycomb appearance (Fig. 2 B), with low hypoenhancement in septa in venous and late phases. Other 4 lesions were able to be detected in venous and late phases as smaller lesions with rim enhancement: 2 in the left hepatic lobe with 20 mm, and 2 in the right hepatic lobe with 40 and 30mm (Fig.2 C).
Blood and faecal cultures were obtained, and the patient was medicated with piperacillin/tazobactam and metronidazole. Puncture aspiration of the largest nodular lesion was performed collecting fluid for culture, but drain placement was not possible. No causal bacteria were identified, either in blood or faecal cultures, or in culture of the aspirated fluid. Furthermore, a biopsy was also performed with a Trucut 18G needle, with histology revealing degenerative alterations, nonspecific reactive inflammatory process and wall of abscess, with a suppurative component of the liver, consisting of fibrin exudate within which necrotic material, cellular remains/debris and numerous inflammatory cells (predominant neutrophil polymorphonuclear leukocytes and cells of the line histiocytic macrophage with debris inside).
One week later a new attempt of percutaneous abscess was performed with drain placement, draining a total of 220 mL of serosanguineous fluid in 72 hours. Revaluation CT and CEUS revealed a decrease in the size of the lesions after 2 weeks of endovenous antibiotic therapy. The patient was evaluated by the hepatobiliary surgery team who advised to maintain medical treatment since the patient did not have indication for surgical treatment.
The patient completed 3 weeks of endovenous piperacillin/tazobactam and metronidazole with fever cessation and negativation of inflammatory parameters. An additional 4 weeks of antibiotic therapy was done with cefixime and metronidazole. The revaluation CT after antibiotic therapy showed residual liver lesions, with significantly decreased dimensions, 1 in the segment V with 35 mm and 1 in the segments VIII with 43 mm.
WHAT IS THE MOST LIKELY DIAGNOSIS?
DISCUSSION
A liver abscess is a pus-filled mass in the liver that can develop from injury to the liver or an intraabdominal infection disseminated from the portal circulation (1),and in some cases the cause of the liver abscess cannot be established. Most liver abscesses are categorized into pyogenic (usually polymicrobial, more commonly E. coli, Klebsiella, Streptococcus, Staphylococcus, and anaerobes) or amoebic (generally caused by Entamoeba histolytica) (2).
The initial test of choice is an abdominal ultrasound (US), which typically shows hyper or hypoechoic lesions with occasional debris or septation. In CEUS and contrast enhanced CT, peripheral enhancement and oedema are not typical but very specific for infection (3). Stains and cultures for aerobes and anaerobes should be obtained from the direct aspirate. Diagnosis is confirmed with positive cultures of fluid aspirated from cystic or solid areas in the liver (2). Blood cultures should be included in the initial laboratory tests to rule out bacteraemia (4).
Treatment includes antibiotic administration and drainage of the abscess, either under US or CT guidance. Empiric antibiotic coverage should cover Enterobacteriaceae, anaerobes, Streptococci, Enterococci, and Entamoeba histolytica, in patients in which the causal organism is unknown (2). The proposed antibiotic regimens include cephalosporins or beta-lactam beta-lactamase inhibitors plus metronidazole, or synthetic penicillins plus aminoglycosides and metronidazole (1, 2). Laparoscopic drainage is required only in patients with peritonitis, ruptured abscess, previously failed drainage procedures and a origin requiring surgery (2).
REFERENCES
- Mischnik A, Kern WV, Thimme R. [Pyogenic liver abscess: Changes of Organisms and Consequences for Diagnosis and Therapy]. Dtsch Med Wochenschr. 2017;142(14):1067-74.
- Akhondi H, Sabih DE. Liver Abscess. StatPearls. Treasure Island (FL): StatPearls Publishing
Copyright © 2022, StatPearls Publishing LLC.; 2022.
- Ahn SJ, Kim JH, Lee SM, Park SJ, Han JK. CT reconstruction algorithms affect histogram and texture analysis: evidence for liver parenchyma, focal solid liver lesions, and renal cysts. Eur Radiol. 2019;29(8):4008-15.
- Rahimian J, Wilson T, Oram V, Holzman RS. Pyogenic liver abscess: recent trends in etiology and mortality. Clin Infect Dis. 2004;39(11):1654-9.
AUTHORS
Ana Isabel Ferreira 1,2,3, Sofia Xavier 1,2,3, Tiago Cúrdia Gonçalves 1,2,3, Sílvia Leite 1,2,3, José Cotter 1,2,3
1 Gastroenterology Department, Hospital Senhora da Oliveira – Guimarães.
2 Life and Health Sciences Research Institute (ICVS), School of Medicine, University of Minho, Braga, Portugal.
3 ICVS/3B’s, PT Government Associate Laboratory, Guimarães/Braga, Portugal.


