US Quiz of the Month – January 2021
CASE REPORT
A 31-year-old Indian patient, living in Europe for the last 7 years, was admitted in the emergency department for jaundice, epigastric and right upper quadrant abdominal pain for the last 3 days, loss of 4.5Kg in the previous month, without fever or other remarkable symptoms. Physical examination showed tenderness on the right upper quadrant and icteric sclera. Laboratory studies revealed normal blood cell counts and C-reactive protein levels (3.5 mg/L), elevated total serum bilirubin levels (5.9 mg/dL), mainly due to direct bilirubin (4.4mg/dL), AST of 107U/L, ALT of 132 U/L, ALP of 354 U/L and GGT of 152 U/L.
Computed tomography (CT) showed a hypodense, multiloculated lesion with cystic areas and calcifications, measuring 7×4.5x7cm, in the pancreatic head, isthmus and body, involving the portal vein and extending to the hepatic hilum, including the main bile duct, without significant upstream dilation (Fig. 1 and 2).

Figure 1. Abdominal CT (axial view): hypodense, multiloculated lesion with cystic areas and calcifications, measuring 7×4.5x7cm, in the pancreatic head, isthmus and body.
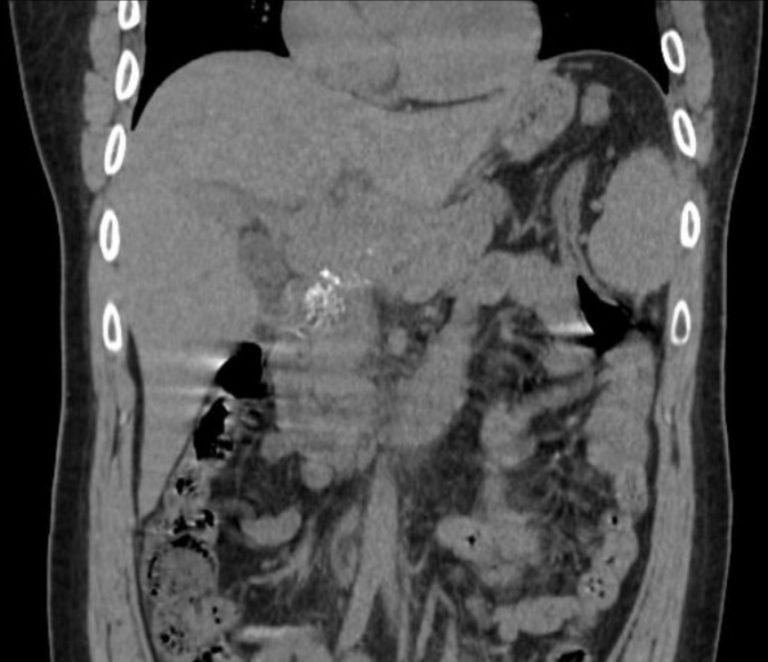
Figure 2. Abdominal CT (coronal view): hypodense, multiloculated lesion with cystic areas and calcifications in the pancreatic head, isthmus and body.
Endoscopic ultrasound (EUS) revealed a hypoechoic retroperitoneal heterogenous lesion, >58mm, with dispersed calcifications, involving the portal vein and distal portion of the bile duct. The lesion contacted the head, isthmus and corpus of the pancreas; the remaining parenchyma and main pancreatic duct appeared normal (Fig. 3 and 4). Fine needle biopsy (22G Cook® ProCore®) was performed with core tissue acquisition.
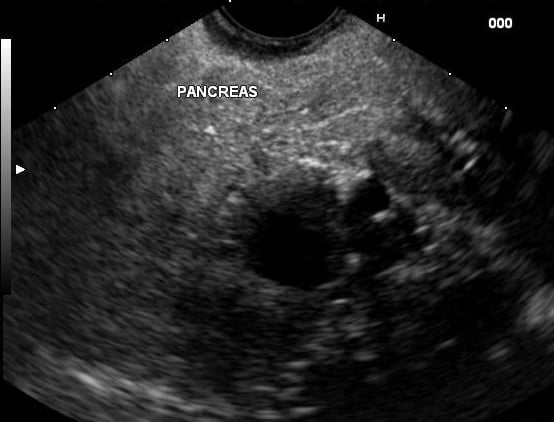
Figure 3. EUS: hypoechoic retroperitoneal heterogenous lesion, with dispersed calcifications, involving the portal vein and distal portion of the bile duct and contacting the head, isthmus and corpus of the pancreas.
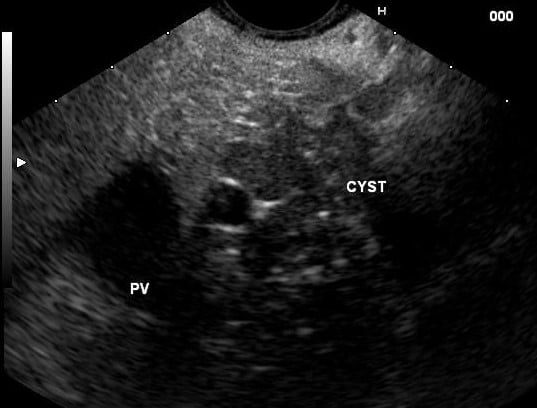
Figure 4. EUS: hypoechoic retroperitoneal heterogenous lesion, with dispersed calcifications, involving the portal vein (PV) and distal portion of the bile duct and contacting the head, isthmus and corpus of the pancreas.
WHAT IS THE MOST LIKELY DIAGNOSIS?
DISCUSSION
Citologic analysis revealed several epithelioid granulomas with caseous necrosis and the presence of giant Langhans cells. Acid-alcohol-resistant bacilli were detected and nucleic acid amplification test positive for Micobacterium tuberculosis complex. The patient was started on tuberculostatic treatment. Thoracic CT did not show typical signs of tuberculosis, there was no history of contacts with other positive patients and immunodeficiency was excluded.1,2
Tuberculosis (TB) is still a common disease worldwide and extra-pulmonary organ involvement reaches 10–15% in immunocompetent patients, of which 11-16% in the gastrointestinal systems. Abdominal TB has concurrent pulmonary disease in only 25%, symptoms are unspecific and vary according to the affected organ, thus, a high index of suspicion is needed. Pancreatic involvement is rare and may present with hypoechoic masses or cystic lesions, mainly in the head or body region, being initially presumed as pancreatic carcinoma in up to 52% of cases, including patients who underwent surgery. Calcifications are typical but may be seen in pancreatic malignancies as well.3 Positive PCR of sampled tissue provides more diagnostic values (47%-96%) than AFB smear (0-62%) and AFB culture (19%-81%).4 However, since extrapulmonary TB is paucibacillary, the yield of organisms is low (<50%) and characteristic histology may be diagnostic, being the presence of caseous granulomas highly suspicious of TB.1, 2
REFERENCES
- Shreshtha S, Ghuliani D. Abdominal tuberculosis: A retrospective analysis of 45 cases. Indian J Tuberc. 2016;63(4):219-224. http://dx.doi.org/10.1016/j.ijtb.2016.09.008.
- García del Olmo N, Boscà Robledo A, Penalba Palmí R, Añón Iranzo E, Aguiló Lucía J. Primary peripancreatic lymph node tuberculosis as a differential diagnosis of pancreatic neoplasia. Rev Española Enfermedades Dig. 2017;109(7):528-530.
- Liang X, Huang X, Yang Q, He J. Calcified peripancreatic lymph nodes in pancreatic and hepatic tuberculosis mimicking pancreatic malignancy. MD J. 2018;0(May):4-8.
- Hoilat GJ, Abdu M, Hoilat J, Gitto L, Bhutta AQ. A Rare Case of Pancreatic Tuberculosis Diagnosed via Endoscopic Ultrasound-Guided Fine Needle Aspiration and Polymerase Chain Reaction. Cureus. 2020;12(of 297).
AUTHORS
Sara Santos1, Diana Carvalho1, Gonçalo Ramos1.
- Gastroenterology Department, Centro Hospitalar Universitário de Lisboa Central, Lisbon, Portugal.


