US Quiz of the Month – Janeiro 2023
CASE REPORT
We present a case of a 78-year-old female patient with a past medical history of arterial hypertension, dyslipidaemia and atrial fibrillation under edoxaban. She was referred to General Surgery department due to a solid pancreatic lesion in a computed tomography (CT) performed in the context of dyspepsia and weight loss, after a normal upper endoscopy. The lesion was described as a solid nodular hypoechogenic lesion with regular margins, measuring approximately 63 x 55 x 65 mm. It was adjacent to the lateral-posterior slope of the pancreatic head, lower border of the liver and infundibular region of the gallbladder and the medial slope of the duodenum, without accurate definition of its origin. It caused a slight posterior deviation of the inferior vena cava and a slight anterior deviation of the splenoportal confluent and biliary tract, keeping these vessels permeable. It did not enhance after intravenous contrast administration, nor had hypervascular behaviour or unequivocal wash out. Laboratory studies were unremarkable.
Endoscopic ultrasound (EUS) (Fig. 1) confirmed a nodular neoformation, hypoechogenic, heterogeneous, with regular and well-defined margins, between the hepatic hilum and the head of the pancreas, but unrelated to both structures. It was apparently encapsulated, Doppler negative, with 65 x 57 mm. No other lesions were identified. EUS-guided fine needle biopsy (EUS-FNB) of the lesion was performed using an 22G needle.
Pathology (Fig. 2) showed sheets of large lymphoid cells with diffuse growth and the immunohistochemical study (Fig. 3) revealed positivity of large lymphoid cells for CD45, CD20, bcl6, MUM1 and PAX-5, multifocal positivity for vimentin and negativity for CD3, CD10 and cytokeratins AE1/AE3 and 8/18; Ki67 immunostaining was high (>50%), favouring a malignant lymphoproliferative neoplastic process of B lymphoid cells with characteristics of diffuse large B cell lymphoma (DLBCL).
The patient was referred to a specialized centre. A contrast-enhanced CT (CeCT) was performed, and no other lesions were found. Additionally, the bone marrow biopsy did not reveal neoplastic involvement. The patient was submitted to chemotherapy protocol with Cyclophosphamide-Doxorubicin-Prednisolone-Rituximab-Vincristine (R-CHOP).
WHAT IS THE MOST LIKELY DIAGNOSIS?
DISCUSSION
Diffuse large B cell lymphoma (DLBCL) is the most common type of non-Hodgkin lymphoma (1) and is more prevalent in elderly patients, mainly in the 7th decade (2). Patients most often present with a rapidly growing tumour mass in single or multiple, nodal or extranodal locations (1).
A morphological diagnosis is required in all cases by immunohistochemistry (IHC) and/or flow cytometry (3). Fluorodeoxyglucose positron emission tomography (FDG-PET) with CT scan is now the gold standard for staging DLBCL patients, since it is more accurate than CeCT, especially in nodal and extranodal sites (3, 4). However, in practice, CeCT is often carried out before FDG-PET/CT (3). Bone marrow biopsy may be avoided when FDG-PET/CT scans demonstrate bone or marrow involvement indicating advanced-stage disease but is appropriate if the PET is negative (5).
Treatment strategies depend on the patients’ age and International Prognostic Index, which includes age, performance status, number of extranodal sites, lactate dehydrogenase value and disease stage according to Ann Arbor staging classification (3).
Figure legends:



Fig. 1 – EUS (transduodenal view) showing a nodular neoformation, hypoechogenic, heterogeneous, with regular and well-defined contours, with 65 x 57 mm (Fig. 1 A); Doppler negative (Fig. 1 B); EUS-FNB (Fig. 1 C).

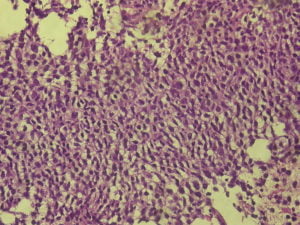

Fig. 2 – Histology compatible with a malignant lymphoproliferative neoplastic process of B lymphoid cells with characteristics of DLBCL, with hematoxylin and eosin stain (Fig. 2 A-C).



Fig. 3 – Immunohistochemical study revealed positivity of large lymphoid cells for CD20 (Fig. 3 A) and bcl6 (Fig. 3 B); Ki67 immunostaining was high (Fig. 3 C), favouring a DLBCL.
REFERENCES
- Li S, Young KH, Medeiros LJ. Diffuse large B-cell lymphoma. Pathology. 2018;50(1):74-87.
- Martelli M, Ferreri AJ, Agostinelli C, Di Rocco A, Pfreundschuh M, Pileri SA. Diffuse large B-cell lymphoma. Crit Rev Oncol Hematol. 2013;87(2):146-71.
- Tilly H, Gomes da Silva M, Vitolo U, Jack A, Meignan M, Lopez-Guillermo A, et al. Diffuse large B-cell lymphoma (DLBCL): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2015;26 Suppl 5:v116-25.
- Barrington SF, Mikhaeel NG, Kostakoglu L, Meignan M, Hutchings M, Müeller SP, et al. Role of imaging in the staging and response assessment of lymphoma: consensus of the International Conference on Malignant Lymphomas Imaging Working Group. J Clin Oncol. 2014;32(27):3048-58.
- Khan AB, Barrington SF, Mikhaeel NG, Hunt AA, Cameron L, Morris T, et al. PET-CT staging of DLBCL accurately identifies and provides new insight into the clinical significance of bone marrow involvement. Blood. 2013;122(1):61-7.
AUTHORS
Ana Isabel Ferreira 1,2,3, Sofia Xavier 1,2,3, Joana Magalhães 1,2,3, Francisca Dias de Castro 1,2,3, Sílvia Leite 1,2,3, José Cotter 1,2,3
Affiliations:
1 Gastroenterology Department, Hospital Senhora da Oliveira – Guimarães.
2 Life and Health Sciences Research Institute (ICVS), School of Medicine, University of Minho, Braga, Portugal.
3 ICVS/3B’s, PT Government Associate Laboratory, Guimarães/Braga, Portugal.


