US Quiz of the Month – March 2021
CASE REPORT
A 48-year-old asymptomatic female underwent an abdominal ultrasound due to liver enzymes elevation (AST 45 U/L, ALT 77 U/L) detected on routine evaluation. Abdominal ultrasound revealed an incidental gastric wall lesion that was misinterpreted as A cyst of the pancreatic body measuring 68x45mm. Additional abdominal computed tomography (CT) was performed showing a well-defined, hypodense gastric mass with calcifications, measuring 65mm, on the posterior wall of the distal body, compressing the transverse colon; no lesions were visible on the pancreas or liver. Upper gastrointestinal endoscopy demonstrated a 6cm rounded subepithelial lesion (SEL), with a central depression, on the posterior face of the distal body of the stomach (Fig. 1).
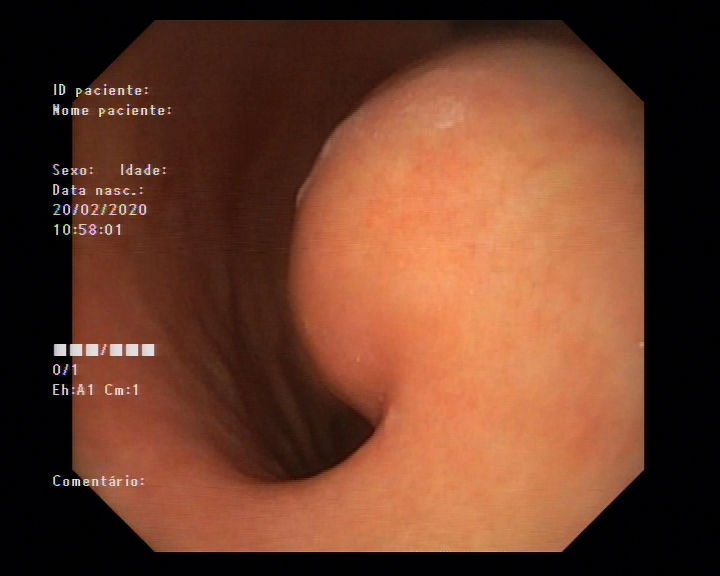
Figure 1. Upper endoscopy: gastric SEL.
On the endoscopic ultrasound (EUS) examination, the gastric lesion corresponded to a well-defined heterogeneous lesion, with solid iso/hypoechoic areas, necrotic/cystic (anechoic) areas and calcifications, located on the fourth layer (muscularis propria) (Fig. 2). Additionally, rounded and hypoechoic perilesional lymph nodes (maximum diameter 14mm) were identified.

Figure 2. EUS: Well-difined heterogeneous with necrotic/cystic areas and calcifications.
EUS-guided fine needle biopsy (FNB) using a 22G needle was performed (two needle passes; AcquireTM Endoscopic Ultrasound FNB Device, Boston Scientific) and the histopathological analyses revealed rare spindle cell tissue fragments, with a fascicular arrangement, without nuclear atypia nor mitosis. Immunohistochemistry staining was positive to S100 and negative to CD117, CD34, DOG 1 and smooth muscle actine (Fig. 3A and 3B).
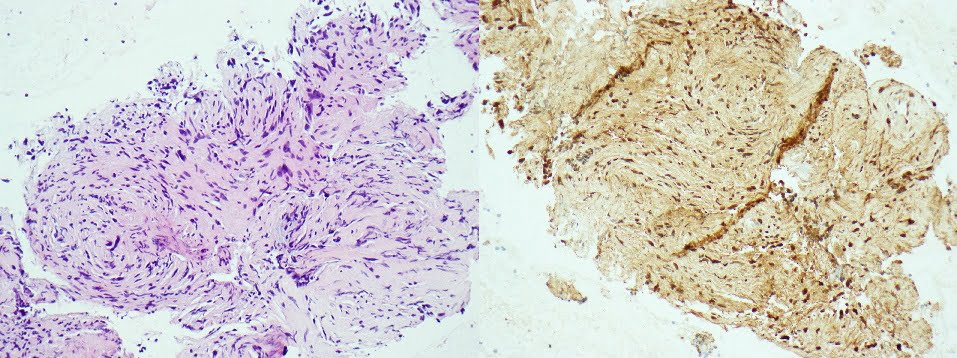
Figure 3. Pathology: A) rare spindle cell tissue fragments, with a fascicular arrangement (HE; 200x); B) positive S100 immunohistochemistry (200x).
WHAT IS THE MOST LIKELY DIAGNOSIS?
DISCUSSION
The histopathological features and immunohistochemical staining pattern were consistent with the diagnosis of gastric schwannoma. After multidisciplinary discussion, the patient was submitted to a laparoscopic partial gastrectomy with Roux-en-Y reconstruction, and the histopathological examination of the surgical specimen confirmed the diagnosis (Fig. 4). Evaluation of 9 lymph nodes revealed reactive follicular hyperplasia.

Figure 4. Resected gastric mass after surgery.
Gastric schwannoma (GS) is a rare neoplasm deriving from Schwann cells of the peripheral nerves in the stomach [1]. It accounts for 0.2% of all gastric tumors and malignant transformation risk is low [1,2]. GS typically grows as a solitary lesion, arising most commonly from the body of the stomach (50%), with a variable size [1,2]. GS can occur at any age but is most frequently noted in the fifth to eight decades, with female predominance [1]. GS is often asymptomatic and can be discovered incidentally on cross-sectional imaging, however it can present with non-specific symptoms [2]. On endoscopy it presents as a SEL with no specific characteristics, corresponding to a hypoechoic lesion located on the third or fourth layers on EUS, undistinguished from other SEL, such as gastrointestinal stromal tumor (GIST) or leiomyoma [3]. As a result, these investigations provide only limited information about the tumor, and the definitive diagnosis is determined after histopathological and immunohistochemical examination, obtained, for example, through EUS-guided FNB [2]. Surgical treatment is considered the treatment of choice in patients with GS [2].
REFERENCES
- Lomdo M, Setti K, Bounaim A et al. Gastric schwannoma: a diagnosis that should be known in 2019. Journal of Surgical Case Reports 2020;1:1-3.
- Mohanty S, Jena K, Bano S, et al. Gastric GIST or gastric schwannoma-a diagnostic dilemma in a young female. International Journal of Surgery Case Reports 2016;28:60-64.
- Faulx A, KothariS, DeWitt J, et al. Guideline: The role of endoscopy in subepithelial lesions in the GI tract. Gastrointestinal Endoscopy 2017;85:1117-1132.
AUTHORS
Catarina Félix1, Joana Veloso Carmo1, Ana Virgínia Araújo2, Rita Vale Rodrigues3, António Martins2, Martinha Chorão4, Beatriz Costa Neves3, Cláudia Branco2, Cristina Chagas1.
- Gastroenterology Department, Centro Hospitalar Lisboa Ocidental, Hospital de Egas Moniz, Lisbon, Portugal.
- Surgery Department, Hospital de Cascais, Cascais, Portugal.
- Gastroenterology Department, Hospital de Cascais, Cascais, Portugal.
- Pathology Department, Centro Hospitalar Lisboa Ocidental, Lisbon, Portugal.


