US Quiz of the Month – Março 2024
Case Report
A 73-year-old male patient with history of depression, thyroidectomy and cholecystectomy presented with intermittent solid-food dysphagia of several years duration with recent worsening. The reported case was not associated with significant weight loss or anorexia. The subject did not report of other symptoms such as regurgitation or chest pain. Physical examination did not reveal anything abnormal and laboratory studies were also within the normal range.
An esophagogastroduodenoscopy was performed showing a subepithelial lesion measuring approximately 15 mm covered with normal and homogeneous mucosa in the proximal esophagus (26cm from the dental arcade). Downstream of this lesion the luminal caliber of the esophagus was narrowed to the cardia and the mucosa was normal.
CT scan revealed concentric thickening of the walls of the middle and distal esophagus to a maximum extent of 14cm, with apparently regular contours. Upstream of the lesion there was ectasia of the esophagus. The findings were corroborated by MRI and esophageal transit, showing a narrowing of the lower two thirds of the esophagus with normal mucosa.
Figure 1.– Esophageal thickening on CT exam (A and B) and MRI (C) and luminal narrowing in esophageal transit (D)
The patient underwent an EUS that revealed in the proximal esophagus an oval formation measuring 15×11 mm, hypoechogenic, homogeneous, depending on the muscular layer, suggestive of leyomioma. Immediately downstream it was observed a diffuse parietal thickening of the esophageal wall until the cardia. The thickening was homogeneous, circumferential, hypoechogenic, originating in the muscular layer reaching a maximum parietal thickening of 15mm.
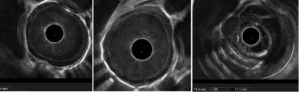
Figure 2. – Esophageal thickening on EUS (A and B) and the proximal oval formation (C).
What is the most likely diagnosis?
Discussion
Those findings were suggestive of diffuse esophageal leiomyomatosis, a benign neoplastic lesion, which was confirmed by cytology needle puncture. Whereas leiomyomas are the most frequent benign tumors of the esophagus, esophageal leiomyomatosis is a rare pathologic entity, more frequent in males, characterized by a circumferential thickening of the muscular layer of the esophageal wall and is known to be associated with nonspecific dysphagia (1). The causes of its incidence are unknown.
Two thirds of the cases of esophageal leiomyomatosis display autosomal dominant transmission, accompanying Alport’s syndrome (a pathologic triad with ocular, renal and auditory impairment) (2).
Irrespective of age at presentation or underlying genetic cause, the extent of esophageal involvement can vary from the entire thoracic esophagus to as little as one-third of the esophageal length, with the distal more often involved than the proximal. Consistent in all cases is circumferential thickening of the muscular layer of the esophageal wall which often results in dysphagia (3).
Achalasia is the main differential diagnosis because of the clinical, radiologic, and endoscopic similarities. The clinical presentation and complementary investigations may sometimes erroneously suggest a malignant tumoral process, particularly when the lesion extends into the fundus (4-5).
This brief report depicts the rare imaging and ultrasound features of diffuse esophageal leiomyomatosis. Herein, we highlight the significance of undertaking a multidisciplinary approach to determine the appropriate treatment regimen, which may end up in an esophagectomy. In a multidisciplinary meeting, it was decided that, for now, the patient would be kept under clinical and endoscopic surveillance.
References
1. Berenguer Francés M, Onrubia Pintado JA, Vázquez Pérez G. [Diffuse esophageal leiomyomatosis as a differential diagnosis of dysphagia] Med Clin (Barc) 2016;147:377–378.
2. Crouch G, Devitt PG, Thompson SK. Diffuse esophageal leiomyomatosis. Dis Esophagus. 2011
3. Figueiredo LM, Rafael MA, Branco JC, Rodrigues CG, Alves AT, Horta D, Martins A. Multidisciplinary Approach to Diagnose and Treat Diffuse Esophageal Leiomyomatosis: A Case Report. Clin Endosc. 2020
4. Milito P, Asti E, Aiolfi A, Zanghi S, Siboni S, Bonavina L. Clinical outcomes of minimally invasive enucleation of leiomyoma of the esophagus and esophagogastric junction. J Gastrointest Surg. 2020
5. Rapp JB, Ciullo S, Mallon MG. Diffuse esophageal leiomyomatosis: A case report with surgical correlation. Clin Imaging. Jul 23.
Authors
André Trigo1 , Margarida Ferreira1, João Almeida2, Francisco Portela1, Pedro Figueiredo1
1 Gastroenterology Department, Centro Hospitalar Universitário da Universidade de Coimbra, Coimbra, Portugal.
2 Surgery Department, Centro Hospitalar Universitário da Universidade de Coimbra, Coimbra, Portugal.


