US Quiz of the Month – Outubro 2022
CASE REPORT
The authors present the case of a 83-year-old man with a computed tomography (CT) scan done for other purposes showing the presence of a hyperenhancing, discretely heterogeneous nodular lesion in the neck of the pancreas, with slightly irregular margins, measuring 30x20mm.
Endoscopic ultrasound (EUS) showed an apparently solid, hypoechoic, well-demarcated but with irregular margins, round, hypervascular lesion, measuring 21x24mm, adjacent to the main pancreatic duct (MPD) though no communication, obstruction or dilation were noticed (Figure 1).
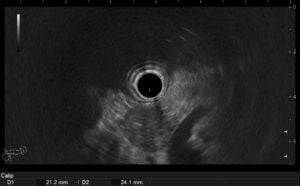
Figure 1
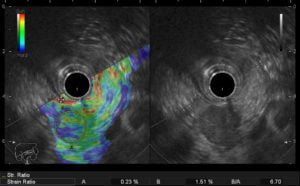
On elastography, a strain ratio of 6.7 was calculated (Figure 2).

Contrast-enhanced ultrasound with SonoVueTM revealed hyperenhancement of the lesion (Figure 3).
WHAT IS THE MOST LIKELY DIAGNOSIS?
MRI revealed a cystic lesion with multiple millimetric cysts separated by filiform septations with mild wall enhancement and no restricted diffusion, establishing a diagnosis of serous cystadenoma.
The histological examination from the FNA sample revealed a scarce specimen for evaluation, with columnar epithelial cells with mild atypia, positive for CK7 and 19, negative for p53, chromogranin A and synaptophysin.
Serous cystadenoma (SCA) is a relatively rare pancreatic neoplasm which accounts for only 2% of pancreatic tumors (1–3). It occurs more commonly in middle-aged or older women and are usually diagnosed incidentally. Patients are generally asymptomatic and SCAs typically follow a benign course (2).
Approximately 40% of pancreatic serous cystadenoma originate from the pancreatic head and uncinate process, while the remainder arise from the pancreatic body or tail (3)
Histologically, they consist of a single layer of cuboidal glycogen-rich cells with round nuclei and clarified cytoplasm (1–3). According to the WHO classification, SCNs are classified into microcystic SCA, macrocystic SCA, solid serous adenoma, von Hippel–Lindau-associated serous cyst neoplasm, and mixed serous–neuroendocrine neoplasm (2). The microcystic type is by far the most described form. The honeycomb microcystic appearance with a central scar is highly suggestive of a serous cystic adenoma and usually no further investigation is required. In rare cases, however, the cysts are so small and crammed together that it presents as a pseudo solid-appearing serous cystic adenoma (1).
Patients with SCA, specially with this pseudo solid-appearance, such as the present case, may have imaging findings that closely resemble those of patients with pancreatic neuroendocrine neoplasms (pNENs), metastatic renal cell carcinoma, solid pseudopapillary tumor or acinar cell carcinomas (1,4). EUS-FNA alone may not accurately differentiate SCA from other pancreatic neoplasms, making the preoperative diagnosis a challenge (1,2), thus leading to unnecessary surgical resections in many cases.
REFERENCES
- Manfrin E, Perini C, di Stefano S, Bernardoni L, Parisi A, Frulloni L, et al. Pseudo solid-appearing pancreatic serous microcystic adenomas: Histologic diagnosis with the EUS core biopsy fork-tip needle. Endosc Ultrasound. 2019 Sep 1;8(5):334–41.
- Nakamura S, Murata Y, Uchida K, Nishikawa K, Iizawa Y, Fujii T, et al. Microcystic serous cystadenoma mimicking pancreatic neuroendocrine neoplasm: report of a resected case with preoperative diagnostic difficulty and review of the literature. Surg Case Rep. 2022 Sep 30;8(1).
- Chu LC, Singhi AD, Haroun RR, Hruban RH, Fishman EK. The many faces of pancreatic serous cystadenoma: Radiologic and pathologic correlation. In: Diagnostic and Interventional Imaging. Elsevier Masson SAS; 2017. p. 191–202.
- Hamid M, Tbouda M, Majbar AM, Raiss M, Ahallat M. Pancreatic solid serous cystadenoma treated by laparoscopy: Presentation of a new case report and review of the literature. Int J Surg Case Rep. 2017;40:97–101.
AUTHORS
Pereira M1, Ramos D1, Caldeira A1, Pestana I1, Banhudo A1
1 – Serviço de Gastrenterologia do Hospital Amato Lusitano – ULS Castelo Branco


