US Quiz of the Month – December 2019
CASE REPORT
A 50-year-old female patient without relevant past medical history was admitted in the emergency department for persisting vomiting and epigastric pain. Laboratory examinations revealed mild leukocytosis (white blood cells 13330 u/L) and hypokalemia (3.21mmol/L). An abdominal computed tomography was performed showing marked dilation of the stomach (Figure 1) related to a ill-defined hypoechogenic mass with 44mm in the transition between the second and third portion of the duodenum (Figure 2).

Figure 1. CT scan showing marked dilation of the stomach
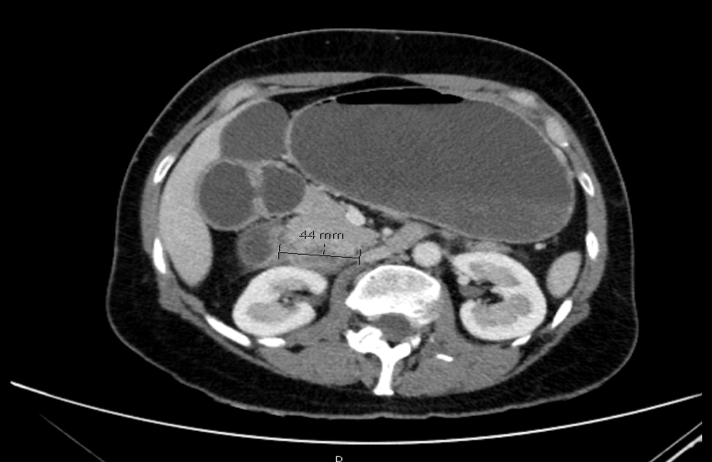
Figure 2. CT scan showing an hypoechogenic mass with 44mm in the transition between the second and third portion of the duodenum.
Upper endoscopy was performed showing a stenosis in the transition between D2 and D3, not transposable with the endoscope with edema of the mucosa, consistent with extrinsic compression (Figure 3).
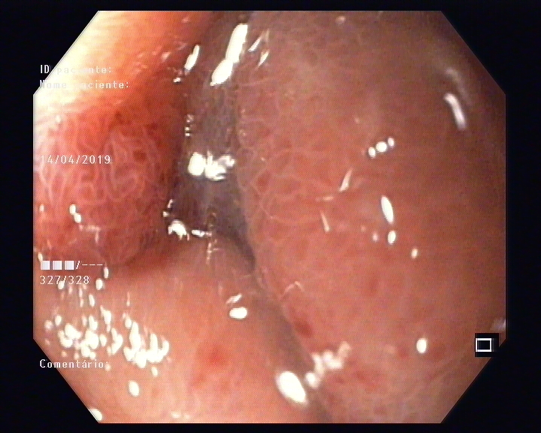
Figure 3. Upper endoscopy showing stenosis in the transition between D2 and D3 with edema of the mucosa.
She was admitted with nasogastric tube placement and parenteral nutrition. Endoscopic ultrasound (EUS) was performed using a linear endoscope showing a hypoechogenic heterogeneous lesion with 37x30mm in relation to the fourth layer of the duodenal wall (Figure 4). The lesion was only observed by EUS in the bulb since it was not possible to transpose the stenosis.
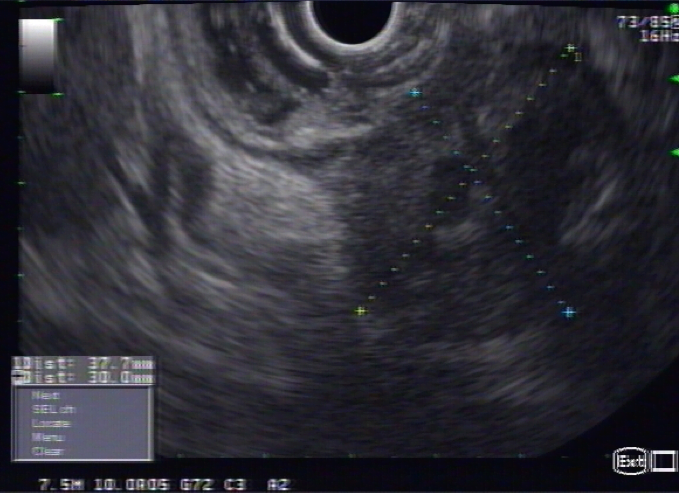
Figure 4. Endoscopic ultrasound showing an hypoechogenic heterogeneous lesion with 37x30mm in relation to the 4th layer of the duodenal wall.
An EUS-guided fine needle aspiration (FNA) was performed with a 22 Gauge needle in 3 passages (Figure 5).
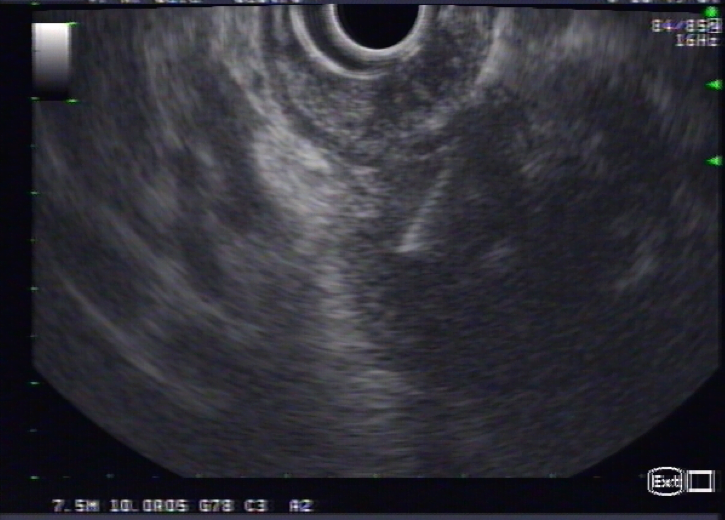
Figure 5. EUS-FNA of the lesion.
WHAT IS THE MOST LIKELY DIAGNOSIS?
DISCUSSION
Cytological exam was compatible with adenocarcinoma and the patient was submitted to a gastroduodenopancreatectomy. Pathologic examination showed an adenosquamous carcinoma of the ampulla of Vater with invasion of the pancreatic parenchyma, the duodenal wall, from the mucosa to the subserosa and lymphovascular and perineural invasion.
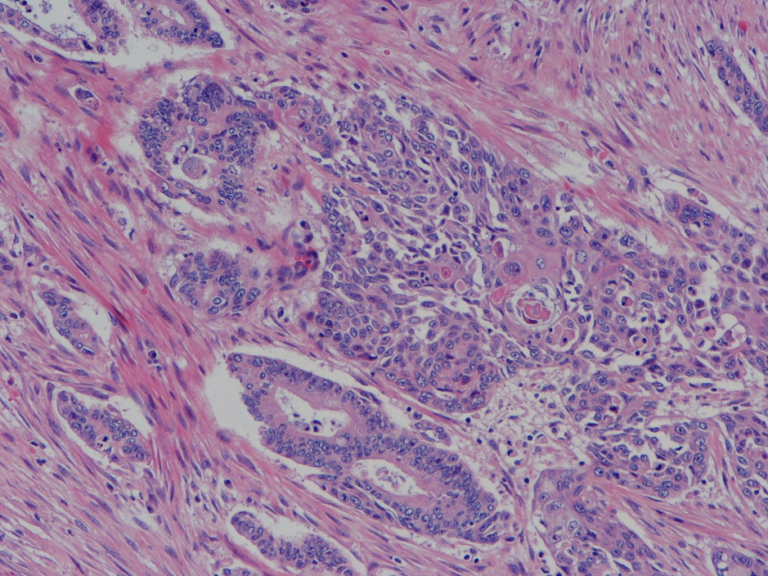
Figure 6. Histology showing adenosquamous carcinoma of the ampulla of Vater with squamous and adenocarcinoma components (H&E, 100x).
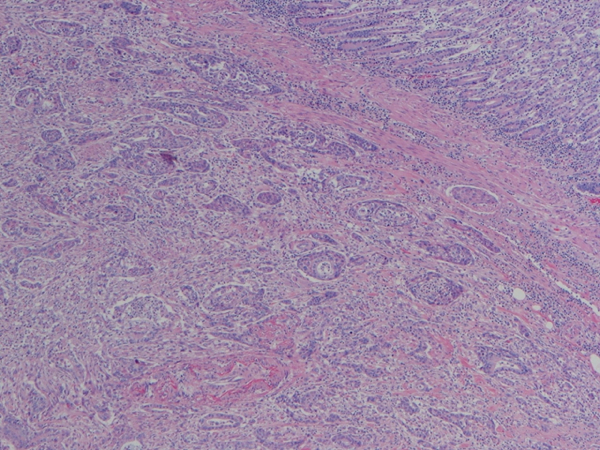
Figure 7. Histology showing adenosquamous carcinoma of the ampulla of Vater with invasion of duodenal wall and lymphovascular and perineural invasion (H&E, 40x).
The margins were free of lesion. The final diagnosis was adenosquamous carcinoma of the ampulla de Vater pT3b N1 LV1 Pn1 R0 and the patient was proposed for chemotherapy.
Adenosquamous carcinoma (ASC) is a rare malignant tumor of the ampulla of Vater characterized by the present of two malignant components including adenocarcinoma and squamous cell carcinoma. The origin of the squamous carcinoma in the ampulla of Vater remains unclear. ASC is considered clinically more aggressive and with poorer prognosis compared to adenocarcinoma but biologic behavior is still unknown due to its rarity, as well as the optimal therapeutic approach.
REFERENCES
- Carvalho et al. Adenosquamous carcinoma of the ampulla of Vater: a rare cause of obstructive jaundice. GE Port J Gastroenterol 2018; 25(4):195
- Hoshimoto et al. Adenosquamous carcinoma of the ampulla of Vater: a case report and literature review. World J Sur Oncol 2015; 13:287
- Lee et al. Adenosquamous carcinoma of the ampulla of Vater – a report of two cases. The Korean Journal of Pathology 2006; 40: 160.
AUTHORS
Mafalda Sousa 1, Sónia Fernandes1, Luísa Proença1, Carlos Fernandes¹, Xiaogan Wen2, Antónia Furtado2, João Carvalho1
- Gastroenterology Department, Centro Hospitalar de Vila Nova de Gaia e Espinho, Portugal
- Pathology Department, Centro Hospitalar de Vila Nova de Gaia e Espinho, Portugal


