US Quiz of the Month – May 2019
CASE REPORT
A 39-year-old female with no significant past medical history presented with intense epigastric, colic pain for the three previous days. Laboratory studies showed mild and isolated C-reactive protein (CRP) elevation (1.9 mg/dL); liver function tests and pancreatic enzymes were within normal range. An abdominal computed tomography (CT) was performed and revealed a duodenal (D2/D3) endophytic polypoid, high density, heterogeneous lesion, with 26 mm; biliary tree and pancreas were normal (Figure 1).
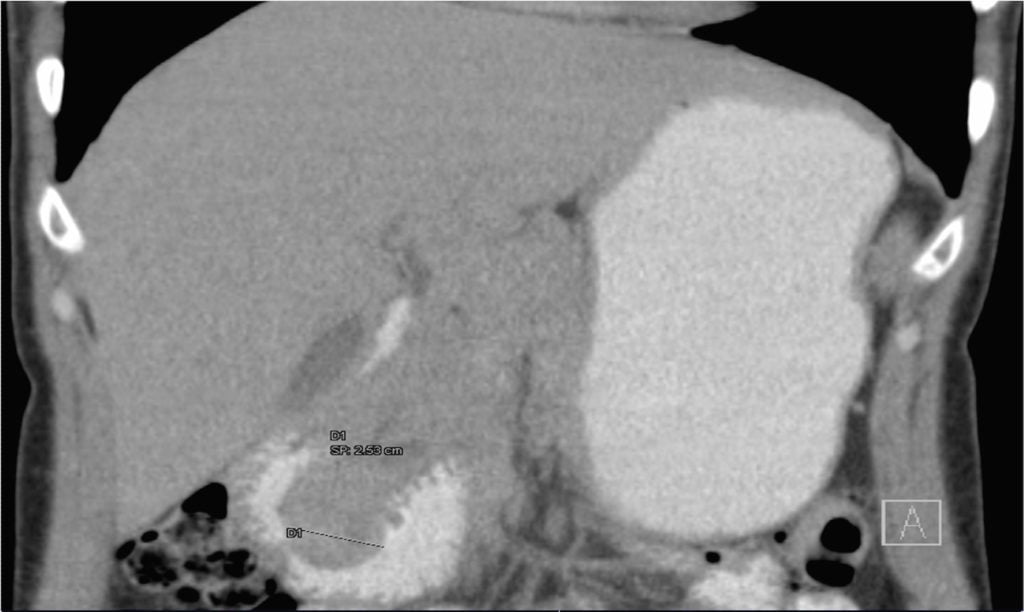
Figure 1. Abdominal CT, coronal view: duodenal (D2/D3) endophytic polypoid, high density, heterogeneous lesion, with 26 mm.
Upper endoscopy (Figure 2A) and duodenoscopy (Figure 2B) identified a 25 mm large subepithelial lesion, distal to the duodenal papilla (black circle in Figure 2A), with ulcerated top. Endoscopic ultrasound (EUS) examination confirmed a peripapillary subepithelial lesion with 22 mm and massively calcified, with posterior acoustic shadowing (transitionzone undefined)(Figure 3); the common bile duct was normal.
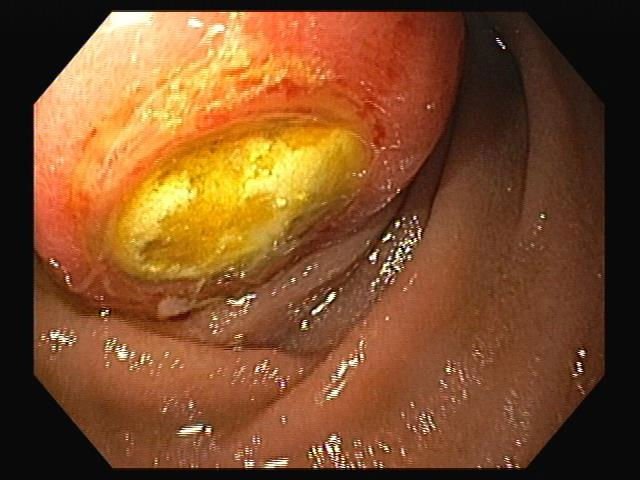
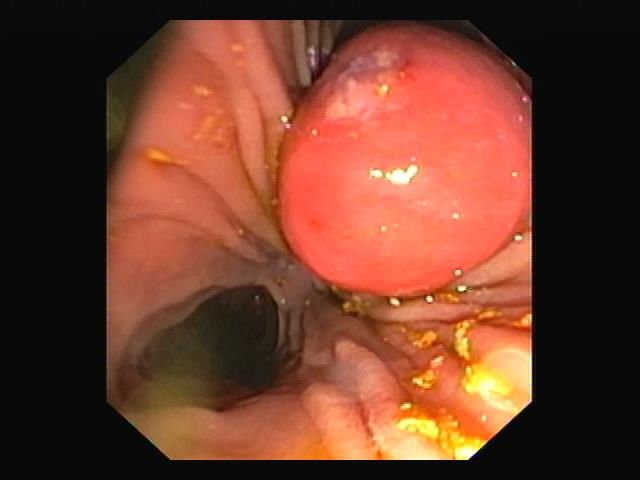
Figure 2. A) Upper endoscopy; B) Duodenoscopy: 25 mm large subepithelial lesion, distal to the duodenal papilla (black circle in Figure 2A), with ulcerated top.
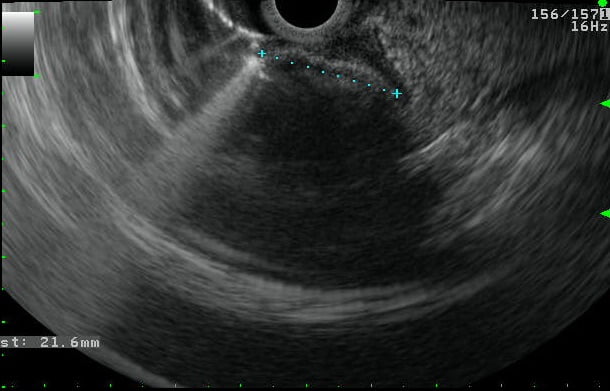
Figure 3. EUS, D2 position: peripapillary subepithelial lesion with 22 mm and massively calcified, with posterior acoustic shadowing.
WHAT IS THE MOST LIKELY DIAGNOSIS?
DISCUSSION
In this patient, EUS findings raised the diagnostic suspicion of a gallstone impacted in the duodenal wall through a peripapillary bilioenteric fistula. Therefore duodenoscopy was repeated at day 6 but instead of the lesion previously seen there was now a large peripappilary orifice, suggestive of a bilioenteric fistula (40 mm large after contrast injection and guide-wire exploration) (Figure 4). There was spontaneous and complete abdominal pain remission in less than a week after admission.

Figure 4. Duodenoscopy, fluoroscopic image: large peripappilary orifice, suggestive of a bilioenteric fistula (guide-wire exploration).
The case presented was particularly challenging as theendoscopic and imagiologic appearance mimicked that of a calcified subepithelial lesion with ulcerated top, such as GIST. Most common subepithelial lesions found in the duodenum are GIST, leyomiomas, lipomas and carcinoids and EUS plays a major role in the differential diagnosis. These lesions may occasionally show calcification, usually focal or punctate.1However, massive calcification is extremely rare (it has been described in a few cases of GIST)1and may point to an alternative diagnosis such as an impacted gallstone into the duodenal wall, particularly if found in D2. There are only three published case reports of parapapillary fistula with impaction of a gallstone into the duodenal wall.2,3
REFERENCES
- Izawa N, Sawada T, Abiko R, Kumon D, Hirakawa M, Kobayashi et al.Gastrointestinal stromal tumor presenting with prominent calcification. World J Gastroenterol.2012;18:5645-8.
- Okabe Y, Kaji R, Ishida Y, Noda T, Sasaki Y, Tsuruta O et al.Successful endoscopic extraction of a large impacted choledocholithiasis in the ampulla of vater: two interesting cases. Dig Endosc. 2010;22:103-6.
- Papanikolaou IS, Polymeros D,KontopoulouC, Chatzilia D, Triantafyllou K.Impaction of a gallstone into the duodenal wall.Endoscopy. 2010;42:297-298.
AUTHORS
Susana Marques 1,2, Miguel Bispo 3, Pedro Pinto-Marques 2,4 , David Serra 2
- Gastroenterology Department, Centro Hospitalar de Lisboa Ocidental, Lisboa, Portugal.
- Gastroenterology Department, Hospital da Luz, Lisboa, Portugal.
- Gastroenterology Department, Fundação Champalimaud, Lisboa, Portugal.
- Gastroenterology Department, Hospital Garcia de Orta, Almada, Portugal.


